Although frequently overlooked, bursitis can have a significant effect on daily living, impeding movement and creating discomfort. This comprehensive guide aims to shed light on the intricacies of bursitis, offering insight into its causes, symptoms, diagnosis, treatment options, and preventive measures. Individuals can better navigate their way to relief and improved mobility by unlocking the mysteries surrounding this condition.
Key questions
To begin with, it is worth listing the key problems that will be discussed in the article:
- What is bursitis and how does it affect the body?;
- What are the common causes of bursitis?;
- Who is at risk of developing bursitis?;
- What are the symptoms of bursitis?;
- How is bursitis diagnosed?;
- What are the treatment options for bursitis?;
- What are the potential consequences of leaving bursitis untreated?;
- How can bursitis be prevented?
What is Bursitis?
Bursitis is a painful condition that affects the small, fluid-filled sacs called bursae, which cushion the bones, tendons, and muscles near joints. These sacs reduce friction and allow smooth movement of the joints. Bursitis occurs when these bursae become inflamed due to repetitive motions, injury, infection, or underlying conditions such as rheumatoid arthritis or gout.
Common symptoms of bursitis include pain, tenderness, swelling, and limited range of motion in the affected joint. The most commonly affected joints are the shoulder, elbow, hip, and knee, although bursitis can occur in any joint.
Treatment for bursitis typically involves resting the affected joint, applying ice packs to reduce inflammation, taking over-the-counter pain relievers, and undergoing physical therapy to strengthen muscles and improve joint function. In severe cases, a doctor may recommend corticosteroid injections to reduce inflammation or, rarely, surgical removal of the inflamed bursa.
Causes
Bursitis can be caused by a variety of factors, including:
- Repetitive Motion: Engaging in repetitive activities or movements that put stress on a particular joint can lead to irritation and inflammation of the bursae over time. This is common in occupations or sports that involve repetitive motions, such as painting, gardening, or playing tennis;
- Trauma or Injury: Direct trauma or injury to a joint can cause inflammation of the bursae. This can occur from a fall, blow, or other impact to the joint area;
- Overuse: Overuse of a joint without adequate rest can lead to bursitis. This often occurs in athletes or individuals who suddenly increase the intensity or duration of their physical activities;
- Infection: Bursitis can sometimes develop as a result of bacterial infection in the bursae, leading to a condition known as septic bursitis. This type of bursitis requires prompt medical attention and treatment with antibiotics;
- Underlying Conditions: Certain underlying medical conditions, such as rheumatoid arthritis, gout, or pseudogout, can increase the risk of developing bursitis. These conditions can cause inflammation throughout the body, including in the bursae;
- Age: As people age, the bursae may become less elastic and more prone to inflammation, increasing the risk of bursitis;
- Poor Posture or Biomechanics: Poor posture or biomechanics can place abnormal stress on joints, leading to bursitis over time. This can occur due to factors such as muscle imbalances, joint misalignment, or structural abnormalities.
It’s essential to identify and address the underlying cause of bursitis to effectively manage symptoms and prevent recurrence. In many cases, modifying activities, improving posture, and incorporating appropriate rest and stretching exercises can help reduce the risk of bursitis.
Who is at risk?
Several factors can increase the risk of developing bursitis. Individuals who fall into the following categories may be at higher risk:
- Occupational Risk: People whose jobs involve repetitive motions or prolonged periods of pressure on particular joints are at increased risk. This includes occupations such as painting, carpentry, plumbing, cleaning, and gardening;
- Athletes: Athletes who participate in sports that involve repetitive motions, sudden movements, or direct impact on joints are at risk. Sports such as tennis, golf, baseball, and running can increase the likelihood of developing bursitis;
- Age: Older adults are more prone to developing bursitis due to changes in joint structure and decreased elasticity of the bursae as they age;
- Medical Conditions: Certain medical conditions, such as rheumatoid arthritis, gout, diabetes, thyroid disorders, and autoimmune diseases, can increase the risk of bursitis;
- Obesity: Excess weight puts additional stress on the joints, increasing the risk of inflammation and bursitis;
- Previous Injuries or Surgery: Individuals who have experienced previous joint injuries or undergone joint surgery may have an increased risk of developing bursitis;
- Poor Posture and Biomechanics: Poor posture, joint misalignment, muscle imbalances, or structural abnormalities can place undue stress on joints, increasing the risk of bursitis;
- Infections: Certain infections, particularly bacterial infections, can lead to septic bursitis, increasing the risk for individuals who have compromised immune systems or who have experienced recent trauma or surgery;
- Genetics: Some individuals may have a genetic predisposition to conditions that affect joint health, which can increase their susceptibility to bursitis.
It’s important for individuals in these high-risk categories to be aware of the signs and symptoms of bursitis and to take preventive measures, such as proper warm-up and stretching before physical activity, maintaining a healthy weight, practicing good posture, and using ergonomic equipment if applicable. Prompt treatment of any underlying medical conditions can also help reduce the risk of developing bursitis.
Symptoms
The symptoms of bursitis can vary depending on the affected joint and the severity of inflammation. However, common signs and symptoms include:
- Pain: Pain is the most prevalent symptom of bursitis. It usually worsens with movement or pressure on the affected joint and may be described as a dull ache, tenderness, or sharp pain;
- Swelling: Inflammation of the bursae can lead to swelling in the affected area, which may be visible or palpable;
- Tenderness: The affected joint may feel tender to the touch, particularly around the bursa;
- Redness: In some cases, the skin over the affected joint may appear red or feel warm to the touch due to increased blood flow and inflammation;
- Stiffness: Bursitis can cause stiffness and limited range of motion in the affected joint, making it difficult to move or perform certain activities;
- Difficulty with Movement: Activities that involve bending, kneeling, or putting pressure on the affected joint may exacerbate symptoms and cause discomfort;
- Pain at Rest: In severe cases, bursitis pain may persist even at rest, particularly if the inflammation is severe or if there is an underlying infection;
- Pain with Specific Movements: Certain movements or positions may aggravate bursitis pain, such as reaching overhead (shoulder bursitis), bending the elbow (elbow bursitis), or squatting (hip or knee bursitis);
- Crepitus: In some cases, bursitis can cause a grating or grinding sensation (crepitus) in the affected joint, particularly if there is associated inflammation of nearby tendons.
It’s important to note that the symptoms of bursitis can overlap with other conditions affecting the joints, such as arthritis or tendonitis. If you experience persistent or severe joint pain, swelling, or difficulty with movement, it’s essential to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
Diagnosis
Diagnosing bursitis typically involves a combination of medical history, physical examination, and possibly imaging studies. Here’s an overview of the diagnostic process:
- Medical History: Your doctor will ask about your symptoms, including when they started, any activities or movements that worsen the pain, and any previous injuries or medical conditions that may be contributing factors;
- Physical Examination: During the physical exam, your doctor will inspect the affected joint for signs of inflammation, such as swelling, tenderness, redness, and warmth They may also assess your range of motion and perform specific tests to help differentiate bursitis from other conditions affecting the joint;
- Imaging Studies: While imaging tests such as X-rays, ultrasound, or MRI scans are not always necessary to diagnose bursitis, they may be ordered in certain cases to rule out other potential causes of joint pain or to assess the extent of inflammation and any associated damage. X-rays can help visualize the bones and rule out fractures or arthritis, while ultrasound or MRI scans can provide detailed images of soft tissues, including the bursae and surrounding structures;
- Aspiration: In cases where infection is suspected (septic bursitis), your doctor may perform a procedure called aspiration, where a small sample of fluid is withdrawn from the affected bursa using a needle. The fluid can then be analyzed in a laboratory to determine if bacteria are present, guiding appropriate treatment;
- Blood Tests: Blood tests may be ordered to check for markers of inflammation or to assess for underlying medical conditions that may predispose you to bursitis, such as rheumatoid arthritis or gout.
Once a diagnosis of bursitis is confirmed, your doctor will work with you to develop a treatment plan tailored to your specific needs and may recommend lifestyle modifications, medications (such as nonsteroidal anti-inflammatory drugs), physical therapy, or other interventions to relieve symptoms and promote healing. In cases of septic bursitis or severe inflammation that does not respond to conservative measures, additional treatments such as corticosteroid injections or, rarely, surgical drainage of the bursa may be considered.
Treatment

The specific treatment approach may vary depending on the severity of symptoms, the underlying cause of bursitis, and individual factors such as age and overall health. Here are some common treatment options:
- Rest and Immobilization: Giving the affected joint adequate rest and avoiding activities that exacerbate symptoms can help reduce irritation and inflammation of the bursa. Immobilizing the joint with a splint or brace may also be beneficial in some cases;
- Ice Therapy: Applying ice packs to the affected area for 15-20 minutes several times a day can help reduce pain and inflammation. Be sure to wrap the ice pack in a thin cloth to protect the skin;
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs such as ibuprofen (Advil, Motrin) or naproxen (Aleve) can help relieve pain and reduce inflammation. Follow the recommended dosage instructions and talk to your doctor before taking any medication, especially if you have underlying health conditions or are taking other medications;
- Physical Therapy: A physical therapist can design a tailored exercise program to strengthen the muscles surrounding the affected joint, improve flexibility, and restore range of motion. They may also use techniques such as ultrasound or massage to help reduce inflammation and promote healing;
- Corticosteroid Injections: In cases of severe or persistent bursitis, your doctor may recommend a corticosteroid injection into the affected bursa to reduce inflammation and alleviate pain. These injections can provide significant relief, but they are typically limited to a few times per year due to potential side effects;
- Ultrasound-Guided Aspiration: If bursitis is caused by infection (septic bursitis), your doctor may perform a procedure called aspiration to drain fluid from the affected bursa and test it for bacteria. Antibiotics may be prescribed if an infection is present;
- Activity Modification: Modifying activities or using ergonomic equipment to reduce strain on the affected joint can help prevent recurrence of bursitis. Your doctor or physical therapist can provide guidance on proper body mechanics and activity modification;
- Surgery: In rare cases where conservative treatments fail to provide relief, surgical removal of the inflamed bursa (bursectomy) may be considered. This is usually reserved for severe or recurrent cases of bursitis that do not respond to other treatments.
It’s important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment recommendations tailored to your specific needs and circumstances. They can help you develop a comprehensive treatment plan to manage symptoms, promote healing, and prevent recurrence of bursitis.
Prevention
Preventing bursitis involves adopting lifestyle habits and practices that reduce the risk of joint irritation and inflammation. Here are some strategies to help prevent bursitis:
- Avoid Overuse: Practice moderation and avoid overexertion of your joints, especially during repetitive activities or sports that place strain on specific joints. Take breaks, vary your activities, and incorporate rest days into your routine to allow your joints time to recover;
- Warm-Up and Stretching: Before engaging in physical activity or exercise, perform a thorough warm-up to increase blood flow to your muscles and joints. Incorporate dynamic stretching exercises to improve flexibility and reduce the risk of injury;
- Use Proper Techniques: Maintain good posture and use proper body mechanics when performing tasks such as lifting, bending, or reaching. Use ergonomic tools and equipment when possible to reduce strain on your joints;
- Gradual Progression: If you’re starting a new exercise program or increasing the intensity of your workouts, do so gradually to give your body time to adapt and avoid overloading your joints;
- Strength and Flexibility Training: Incorporate strength training exercises into your fitness routine to strengthen the muscles surrounding your joints and improve joint stability. Focus on exercises that target the muscles supporting the affected joint. Additionally, include flexibility exercises to maintain joint mobility and range of motion;
- Maintain a Healthy Weight: Excess weight puts added stress on your joints, increasing the risk of bursitis and other joint problems. Maintain a healthy weight through a balanced diet and regular exercise to reduce strain on your joints;
- Protective Gear: When engaging in activities that pose a risk of joint injury, such as sports or manual labor, use appropriate protective gear such as knee pads, elbow pads, or supportive braces to cushion and stabilize your joints;
- Listen to Your Body: Pay attention to any early warning signs of joint discomfort or inflammation, such as pain, swelling, or stiffness. If you experience these symptoms, take appropriate measures such as resting, icing the affected area, and modifying your activities to prevent further irritation;
- Stay Hydrated: Proper hydration is essential for maintaining joint health and lubrication. Drink plenty of water throughout the day to support joint function and prevent dehydration;
- Regular Check-Ups: Schedule regular check-ups with your healthcare provider to monitor your joint health, address any underlying medical conditions that may increase your risk of bursitis, and receive guidance on preventive measures tailored to your individual needs.
Bursitis presents a significant challenge for many individuals, disrupting their daily activities and diminishing their quality of life. However, armed with knowledge about its causes, symptoms, and treatment options, individuals can take proactive steps to manage and alleviate their symptoms effectively. By incorporating preventive measures and seeking timely medical intervention, individuals can mitigate the impact of bursitis on their well-being, enabling them to lead active and fulfilling lives free from the constraints of pain and inflammation.
FAQ
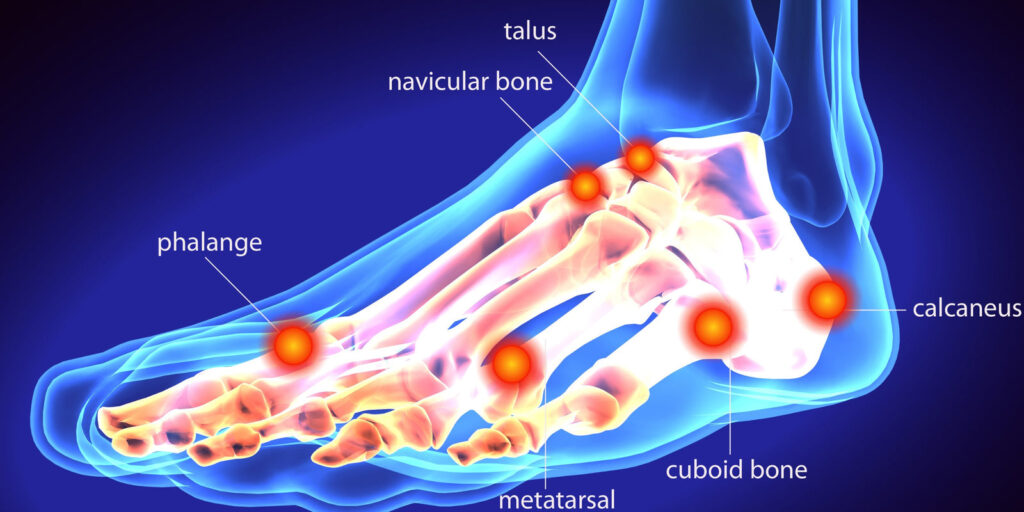
Treating bursitis in the foot typically involves a combination of self-care measures, conservative treatments, and in some cases, medical interventions.
It’s important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment recommendations tailored to your specific needs and circumstances. They can help you develop a comprehensive treatment plan to manage symptoms, promote healing, and prevent recurrence of bursitis in the foot.
In some cases, mild bursitis may resolve on its own with rest and self-care measures. However, the duration and likelihood of spontaneous resolution depend on factors such as the underlying cause, severity of symptoms, and effectiveness of self-care interventions.
While some cases of bursitis may resolve without medical intervention, it’s crucial to monitor your symptoms closely and seek medical attention if they persist or worsen. Early diagnosis and appropriate treatment can help alleviate pain, reduce inflammation, and promote healing, improving your overall quality of life and preventing long-term complications.