Athlete’s foot, corns, calluses, bunions, ingrown toenails, and plantar fasciitis—these are just a few examples of the common foot problems that many individuals encounter at some point in their lives. While often considered minor nuisances, these conditions can cause significant discomfort, pain, and limitation in mobility if left untreated. Understanding the causes, symptoms, and treatment options for these foot ailments is essential for maintaining foot health and overall well-being.
Blisters
Typically caused by friction, heat, or irritation, blisters are fluid-filled sacs that form on the skin. Although often minor, they can be painful and interfere with daily activities. Knowing the causes, prevention, and treatment options can help you treat blistering effectively.
Causes of Blisters:
- Friction: Continuous rubbing or pressure on the skin, commonly from ill-fitting footwear or repetitive movements, can create friction and lead to blister formation;
- Heat: Excessive heat, such as prolonged exposure to the sun or hot surfaces, can cause the skin to blister, especially in areas with less protection, like the feet;
- Moisture: Prolonged exposure to moisture, such as sweaty socks or wet shoes, softens the skin and increases susceptibility to blister formation, particularly during physical activity;
- Irritation: Chemical irritants or allergic reactions can trigger blister formation on the skin, especially if the skin’s protective barrier is compromised.
Prevention of Blisters:
- Proper Footwear: Choose well-fitting shoes with ample toe room and cushioning to minimize friction and pressure on the feet. Avoid wearing new or tight-fitting shoes for extended periods, especially during vigorous activities;
- Moisture Management: Keep feet dry by wearing moisture-wicking socks and breathable shoes. Change socks regularly, especially during intense physical activity or in hot weather, to reduce moisture buildup;
- Protective Measures: Apply moleskin, blister pads, or athletic tape to areas prone to blistering before engaging in activities that may cause friction. These protective barriers help reduce rubbing and prevent blister formation;
- Foot Care: Keep toenails trimmed and skin moisturized to maintain healthy foot hygiene. Avoid harsh chemicals or irritants that may compromise the skin’s integrity.
Treatment of Blisters:
- Leave Intact: If a blister forms, avoid puncturing or popping it, as this increases the risk of infection. Instead, gently clean the area with mild soap and water and cover it with a sterile bandage or blister pad to protect against further irritation;
- Pain Relief: Over-the-counter pain relievers like ibuprofen or acetaminophen can help alleviate discomfort associated with blisters. Avoid applying ice directly to the blister, as this can damage the skin further;
Allow the blister to heal naturally, keeping it clean and protected with a bandage until it resolves on its own. If the blister is large, painful, or shows signs of infection, consult a healthcare professional for proper evaluation and treatment.
Plantar Fasciitis

Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia – a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes. This ailment often manifests as stabbing pain in the heel, particularly noticeable during the first steps in the morning or after prolonged periods of rest. Understanding the causes, effective management strategies, and preventive measures for plantar fasciitis can help alleviate discomfort and promote long-term foot health.
Causes of Plantar Fasciitis:
- Overuse or Strain: Repetitive activities that put excessive stress on the plantar fascia, such as running, walking long distances, or standing for extended periods, can lead to micro-tears and inflammation;
- Biomechanical Issues: Abnormal foot mechanics, such as flat feet, high arches, or improper gait patterns, can alter the distribution of weight and increase the strain on the plantar fascia.
- Tight Muscles: Tight calf muscles or Achilles tendons can pull on the heel bone, causing tension and inflammation in the plantar fascia;
- Obesity or Weight Gain: Excess body weight increases the pressure on the feet and can exacerbate plantar fasciitis symptoms;
- Improper Footwear: Wearing shoes with inadequate support, worn-out soles, or insufficient cushioning can contribute to plantar fasciitis by placing undue stress on the plantar fascia.
Management and Treatment:
- Rest and Ice: Resting the affected foot and applying ice packs can help reduce inflammation and alleviate pain. Ice therapy should be applied for 15-20 minutes several times a day, especially after physical activity;
- Stretching Exercises: Regular stretching of the calf muscles, Achilles tendon, and plantar fascia can improve flexibility and reduce tension. Simple exercises like calf stretches, towel stretches, and toe curls can be beneficial;
- Orthotic Inserts: Custom or over-the-counter orthotic inserts provide arch support, cushioning, and alignment correction, which can alleviate pressure on the plantar fascia and promote proper foot mechanics;
- Night Splints: Wearing a night splint that keeps the foot in a dorsiflexed position can help stretch the plantar fascia and Achilles tendon while sleeping, reducing morning pain and stiffness;
- Physical Therapy: A physical therapist can recommend specific exercises, techniques, and modalities to strengthen the foot muscles, improve flexibility, and address biomechanical issues contributing to plantar fasciitis;
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help reduce pain and inflammation associated with plantar fasciitis. However, these should be used under medical supervision and for short-term relief.
Preventive Measures:
- Proper Footwear: Choose shoes with adequate arch support, cushioning, and shock absorption to reduce strain on the plantar fascia. Replace worn-out shoes regularly and avoid going barefoot on hard surfaces;
- Gradual Activity Progression: Gradually increase the intensity and duration of physical activities to prevent overuse injuries. Incorporate rest days and cross-training activities to minimize repetitive stress on the feet;
- Maintain Healthy Weight: Maintain a healthy weight through a balanced diet and regular exercise to reduce the strain on the feet and lower the risk of developing plantar fasciitis;
- Stretching Routine: Incorporate daily stretching exercises for the calf muscles, Achilles tendon, and plantar fascia into your routine, especially before and after exercise or periods of prolonged standing.
Pay attention to early signs of foot discomfort or pain and address them promptly. Avoid pushing through pain and seek medical attention if symptoms persist or worsen.
Bunions

Bunions are a common foot deformity characterized by a bony bump that forms at the base of the big toe. This condition, medically known as hallux valgus, can cause discomfort, pain, and difficulty wearing certain types of shoes. Understanding the underlying causes, recognizing symptoms, and exploring treatment options can help individuals manage bunions effectively and maintain foot health.
Causes of Bunions:
- Genetics: Bunions often have a hereditary component, with certain foot shapes and structures predisposing individuals to develop this condition;
- Footwear: Wearing tight, narrow, or high-heeled shoes can increase pressure on the toes and contribute to the development of bunions over time;
- Foot Mechanics: Abnormal foot mechanics, such as overpronation (excessive inward rolling of the foot) or flat feet, can alter the distribution of weight and lead to bunion formation;
- Inflammatory Conditions: Certain inflammatory conditions, such as rheumatoid arthritis, can exacerbate joint inflammation and contribute to the progression of bunions;
- Trauma or Injury: Trauma or injury to the foot, such as stubbing the toe or repetitive stress from sports activities, can accelerate the development of bunions.
Symptoms of Bunions:
- Bony Bump: A visible bump at the base of the big toe, which may be red, swollen, or tender to the touch;
- Toe Misalignment: The big toe may angle inward toward the other toes, causing crowding and overlapping of the smaller toes;
- Pain and Discomfort: Bunions can cause pain or soreness, especially when wearing tight or constrictive shoes, walking, or standing for extended periods;
- Limited Mobility: As the bunion progresses, stiffness or restricted movement in the big toe joint may occur, affecting mobility and balance;
- Skin Irritation: Friction from shoes rubbing against the bunion can lead to skin irritation, blisters, or calluses in the affected area.
Treatment Options:
- Footwear Modification: Wear shoes with a wide toe box and adequate arch support to reduce pressure on the bunion and provide comfort. Avoid high heels or shoes with narrow, pointy toes that exacerbate bunion symptoms;
- Padding and Orthotics: Use bunion pads, cushions, or orthotic inserts to cushion the bony protrusion, redistribute pressure, and improve foot alignment. These devices can alleviate pain and prevent further progression of the bunion;
- Toe Spacers and Splints: Toe spacers or splints can help realign the toes, relieve pressure on the bunion, and promote proper toe alignment over time, especially when worn at night;
- Physical Therapy: A physical therapist can recommend exercises and stretches to strengthen foot muscles, improve flexibility, and correct biomechanical issues contributing to bunions;
- Medication: Over-the-counter pain relievers like ibuprofen or acetaminophen can help alleviate pain and inflammation associated with bunions. In some cases, corticosteroid injections may be prescribed to reduce inflammation and provide temporary relief.
If conservative treatments fail to alleviate symptoms or the bunion becomes severe and interferes with daily activities, surgical correction may be considered. Bunion surgery aims to realign the toe joint, remove the bony prominence, and restore normal foot function.
Ingrown Toenails

Ingrown toenails occur when the edge of a toenail grows into the surrounding skin, leading to pain, swelling, and potential infection. This common foot condition can cause significant discomfort and may require prompt attention to prevent complications. Understanding the causes, recognizing symptoms, and exploring treatment options can help individuals manage ingrown toenails effectively and promote healing.
Causes of Ingrown Toenails:
- Improper Nail Trimming: Cutting toenails too short or rounding the edges instead of cutting straight across can encourage the nail to grow into the skin;
- Tight Footwear: Wearing shoes that crowd the toes or exert pressure on the toenails can increase the risk of ingrown toenails by pushing the nail into the surrounding skin;
- Trauma or Injury: Stubbing the toe, dropping heavy objects on the foot, or repetitive activities that cause trauma to the toenail can lead to ingrown toenails;
- Genetics: Some individuals may have inherited traits that predispose them to develop ingrown toenails, such as curved or irregularly shaped nails;
- Poor Foot Hygiene: Inadequate foot hygiene, such as not keeping the feet clean and dry or neglecting to trim toenails properly, can contribute to ingrown toenail formation.
Symptoms of Ingrown Toenails:
- Pain and Tenderness: The affected toe may become tender, swollen, or painful, especially when pressure is applied or when wearing shoes;
- Redness and Swelling: The surrounding skin may appear red, swollen, or inflamed, indicating an inflammatory response to the ingrown toenail;
- Infection: If left untreated, ingrown toenails can become infected, leading to pus or drainage, increased pain, and possible fever or chills;
- Difficulty Walking: Severe ingrown toenails can impair mobility and make it difficult to walk or wear shoes comfortably;
- Nail Changes: The affected toenail may appear curved, jagged, or distorted, with visible signs of ingrowth into the surrounding skin.
Treatment Options:
- Soaking: Soak the affected foot in warm, soapy water several times a day to help soften the skin and reduce inflammation. Epsom salt or mild antiseptic solutions can be added to the water for added benefit;
- Proper Nail Trimming: Trim toenails straight across, avoiding rounded edges, and ensure that the nails are kept at a moderate length to prevent ingrowth into the skin;
- Cotton or Dental Floss: Gently lift the ingrown edge of the toenail with a small piece of cotton or dental floss inserted beneath the nail to encourage it to grow above the skin;
- Antibiotic Ointment: Apply an over-the-counter antibiotic ointment to the affected area to prevent infection and promote healing. Cover the toe with a sterile bandage to keep it clean and protected;
- Pain Relief: Over-the-counter pain relievers like ibuprofen or acetaminophen can help alleviate pain and discomfort associated with ingrown toenails. Follow the recommended dosage instructions;
- Professional Treatment: If home remedies are ineffective or if the ingrown toenail is severe, infected, or recurrent, seek professional treatment from a podiatrist or healthcare provider. They may perform a minor procedure to remove the ingrown portion of the nail or prescribe antibiotics for infection.
Preventive Measures:
- Proper Foot Hygiene: Keep feet clean and dry, paying attention to the areas around the toenails. Trim toenails straight across and avoid cutting them too short;
- Wear Proper Footwear: Choose shoes with adequate toe room and avoid tight or constrictive footwear that puts pressure on the toes;
- Protective Padding: Use protective padding or cushioning around the toenails, especially during physical activity or when wearing tight shoes, to reduce friction and pressure on the nails;
- Regular Foot Exams: Inspect the feet regularly for signs of ingrown toenails or other foot problems, and seek prompt treatment if any issues arise.
Avoid biting or picking at the nails, as this can damage the surrounding skin and increase the risk of ingrown toenails.
Corns and Calluses
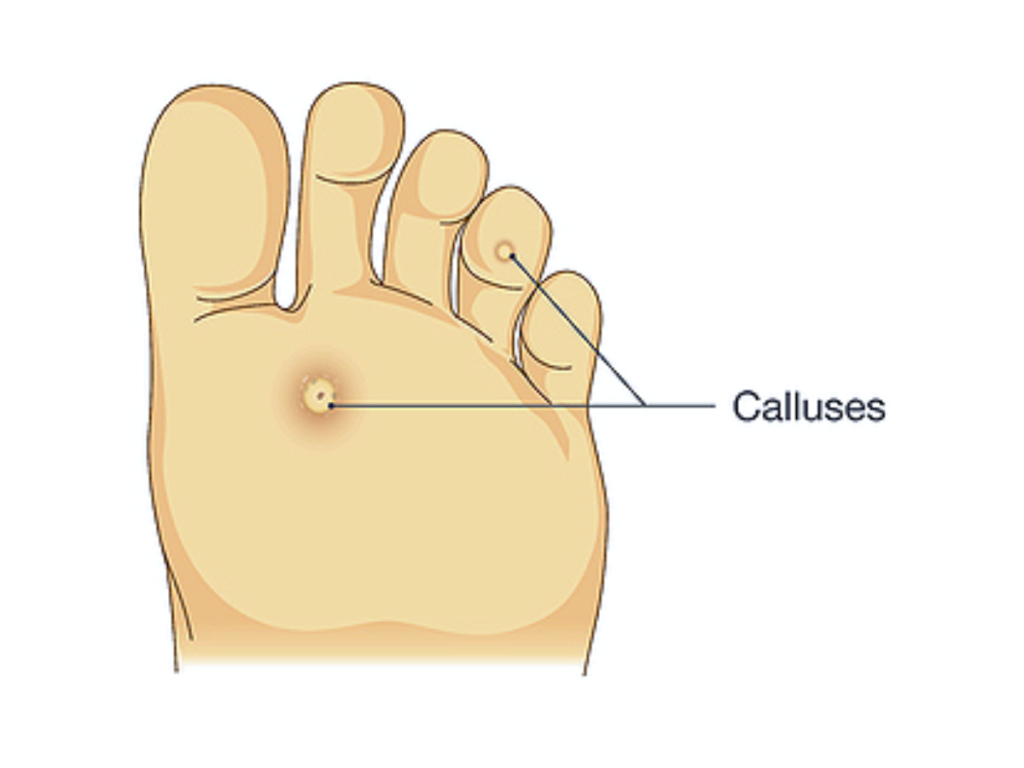
Corns and calluses are thickened areas of skin that develop in response to repeated friction or pressure, often occurring on the feet and hands. While generally harmless, they can cause discomfort and pain if left untreated. Understanding the underlying causes, implementing preventive measures, and exploring treatment options can help individuals manage corns and calluses effectively and maintain healthy skin.
Causes of Corns and Calluses:
- Friction and Pressure: Continuous rubbing or pressure on specific areas of the skin, typically from ill-fitting footwear, repetitive movements, or manual labor, can lead to the formation of corns and calluses;
- Footwear: Wearing shoes with tight or narrow toe boxes, high heels, or seams that rub against the skin can contribute to the development of corns and calluses, especially on the toes, heels, and balls of the feet;
- Biomechanical Issues: Abnormal foot mechanics, such as flat feet, high arches, or toe deformities, can alter the distribution of weight and increase pressure on certain areas of the feet, predisposing individuals to corns and calluses;
- Activities and Occupation: Activities that involve repetitive motions or prolonged standing, such as running, dancing, or working in professions that require manual labor, can increase the risk of developing corns and calluses;
- Age and Skin Conditions: As individuals age, the skin naturally becomes thicker and less elastic, making them more susceptible to corns and calluses. Certain skin conditions, such as dry skin or eczema, can also contribute to the formation of these thickened areas.
Prevention of Corns and Calluses:
- Proper Footwear: Choose shoes with adequate room for the toes, a wide toe box, and cushioning insoles to reduce friction and pressure on the feet. Avoid wearing shoes with high heels or tight-fitting footwear for extended periods;
- Foot Hygiene: Keep feet clean and dry, and moisturize regularly to prevent dry, cracked skin, which can contribute to the formation of corns and calluses;
- Protective Padding: Use cushioning pads or moleskin to protect vulnerable areas of the feet from friction and pressure, especially if engaging in activities that increase the risk of corns and calluses;
- Regular Foot Exams: Inspect the feet regularly for signs of corns, calluses, or other foot problems, and address any issues promptly to prevent worsening or complications;
- Orthotic Inserts: Consider using orthotic inserts or custom-made shoe inserts to provide additional support, cushioning, and alignment correction, which can help reduce pressure on the feet and prevent corns and calluses.
Treatment Options:
- Soaking and Exfoliation: Soak the affected area in warm, soapy water to soften the skin, then gently exfoliate with a pumice stone or foot file to remove dead skin and reduce the thickness of corns and calluses;
- Moisturization: Apply moisturizing creams or lotions to the affected areas regularly to keep the skin soft and hydrated, reducing the risk of further friction and irritation;
- Padding and Cushioning: Use cushioning pads or felt patches to protect corns and calluses from friction and pressure, especially when wearing shoes or engaging in activities that exacerbate symptoms;
- Salicylic Acid Treatment: Over-the-counter products containing salicylic acid can help soften corns and calluses and promote their gradual removal. Follow the product instructions carefully and avoid using on open or infected skin.
If corns and calluses are severe, painful, or recurrent, seek professional care from a podiatrist or healthcare provider. They may perform minor procedures, such as debridement or trimming of thickened skin, to alleviate discomfort and prevent complications.
Athlete’s Foot
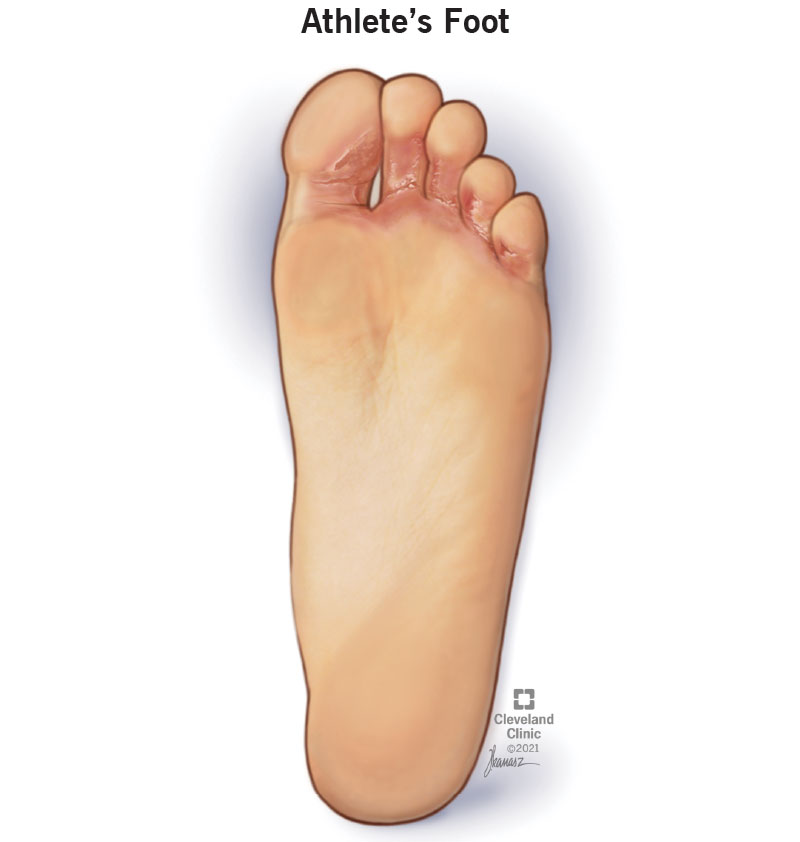
Athlete’s foot, also known as tinea pedis, is a common fungal infection that affects the skin of the feet, particularly between the toes. This contagious condition can cause discomfort, itching, and irritation, and if left untreated, it can lead to further complications. Understanding the causes, recognizing symptoms, and exploring treatment options can help individuals manage athlete’s foot effectively and promote healing.
Causes of Athlete’s Foot:
- Fungal Infection: Athlete’s foot is primarily caused by dermatophyte fungi, which thrive in warm, moist environments such as locker rooms, public showers, and swimming pools. These fungi can infect the skin of the feet upon contact, leading to the development of athlete’s foot;
- Poor Foot Hygiene: Inadequate foot hygiene, such as not drying the feet thoroughly after bathing or wearing damp socks and shoes, can create an ideal environment for fungal growth and increase the risk of athlete’s foot;
- Contaminated Surfaces: Direct contact with contaminated surfaces or objects, such as towels, socks, shoes, or floors in public areas, can transmit the fungal spores responsible for athlete’s foot from person to person;
- Weakened Immune System: Individuals with weakened immune systems, such as those with diabetes, HIV/AIDS, or other medical conditions, may be more susceptible to fungal infections like athlete’s foot;
- Shared Footwear: Sharing shoes, socks, or footwear with an infected individual can facilitate the spread of athlete’s foot and increase the risk of contracting the infection.
Symptoms of Athlete’s Foot:
- Itching and Burning: Athlete’s foot typically presents as itching, burning, or stinging sensations between the toes, particularly after removing socks or shoes;
- Redness and Inflammation: The affected skin may appear red, swollen, and inflamed, with visible signs of irritation and peeling;
- Cracking and Scaling: The skin may become dry, cracked, or scaly, especially in severe cases of athlete’s foot;
- Blisters and Ulcers: Fluid-filled blisters or ulcers may develop on the feet, particularly between the toes, which can be painful and prone to infection;
- Odor: Athlete’s foot can cause a foul odor to emanate from the feet due to bacterial overgrowth and fungal infection.
Treatment Options:
- Antifungal Medications: Topical antifungal creams, sprays, or powders containing ingredients such as clotrimazole, terbinafine, or miconazole are commonly used to treat athlete’s foot. These medications help eradicate the fungal infection and relieve symptoms;
- Antifungal Foot Soaks: Soaking the feet in a solution of diluted antifungal agents, such as vinegar or tea tree oil, can help alleviate itching, reduce inflammation, and inhibit fungal growth;
- Keep Feet Dry: Keep the feet clean, dry, and well-ventilated to discourage fungal growth. Avoid wearing damp socks or shoes and change them regularly, especially after physical activity or exposure to moisture;
- Foot Hygiene: Practice good foot hygiene by washing the feet daily with soap and water, paying special attention to the spaces between the toes. Dry the feet thoroughly, especially between the toes, before putting on socks or shoes;
- Avoid Sharing Footwear: Refrain from sharing shoes, socks, or footwear with others, especially if they have signs of fungal infection. Use protective footwear in public areas such as locker rooms or swimming pools;
- Medical Evaluation: If symptoms persist or worsen despite home treatment, or if there are signs of secondary bacterial infection, seek medical evaluation from a healthcare professional. They may prescribe oral antifungal medications or recommend additional treatment options.
Preventive Measures:
- Wear Breathable Footwear: Choose shoes made of breathable materials such as leather or mesh to allow air circulation and reduce moisture buildup, which can promote fungal growth;
- Use Foot Powder: Apply antifungal foot powder or talcum powder to the feet and inside shoes to absorb moisture and inhibit fungal growth;
- Rotate Shoes: Alternate between different pairs of shoes to allow them to air out and dry completely between wearings, reducing the risk of fungal contamination;
- Practice Good Foot Hygiene: Wash and dry the feet thoroughly, especially between the toes, and avoid walking barefoot in public areas where fungal spores may be present.
Wear properly fitting shoes with adequate room for the toes to prevent excessive friction and pressure on the feet, which can contribute to the development of an athlete’s foot.
Conclusion
Addressing common foot problems such as athlete’s foot, corns, calluses, bunions, ingrown toenails, and plantar fasciitis requires a multifaceted approach that encompasses preventive measures, prompt recognition of symptoms, and appropriate treatment interventions. By understanding the underlying causes and risk factors associated with these conditions, individuals can take proactive steps to mitigate their impact and maintain foot health.
From adopting proper foot hygiene practices and wearing suitable footwear to seeking timely medical evaluation and treatment, there are numerous strategies available to manage and alleviate the discomfort and pain associated with common foot problems. Whether through home remedies, over-the-counter treatments, or professional interventions, it is crucial to prioritize foot health and address any concerns promptly to prevent complications and promote healing.
By incorporating the insights and recommendations provided in this guide into your daily routine, you can empower yourself to take control of your foot health and enjoy a life free from the limitations imposed by common foot problems. Remember, your feet are the foundation of your mobility and well-being – investing in their care and maintenance is an investment in your overall health and quality of life.


