Joint Hypermobility Syndrome is a condition that affects a significant portion of the population, characterized by increased flexibility in the joints beyond what is considered normal.
Key Questions Addressed in the Article:
- What is Joint Hypermobility Syndrome and how does it differ from general joint hypermobility?;
- What are the symptoms of Joint Hypermobility Syndrome and how do they impact daily activities?;
- What are the causes of Joint Hypermobility Syndrome, including genetic predispositions and collagen defects?;
- What are the risk factors associated with developing Joint Hypermobility Syndrome, such as family history and gender disparities?;
- How is Joint Hypermobility Syndrome diagnosed, and what diagnostic tools are commonly used?;
- What treatment options are available for managing Joint Hypermobility Syndrome, including physical therapy, orthotic devices, and surgical interventions?
Unraveling Joint Hypermobility Syndrome: An In-depth Look
Joint Hypermobility Syndrome, often abbreviated as JHS, is a condition related to the connective tissues that play a fundamental role in supporting our bodily structures. One vital component of these tissues is ligaments. These thick bands are the joints’ guardians, safeguarding them from excessive movements, thereby maintaining their stability. However, in individuals diagnosed with JHS, these ligaments exhibit more elasticity and, unfortunately, decreased strength. This leads to the manifestation of exceptionally flexible joints, which, if accompanied by discomfort or pain, could be indicative of JHS.
Recognizing the Signs of Joint Hypermobility Syndrome
While JHS is commonly characterized by pronounced joint flexibility and pain in the muscular structures, the syndrome is notoriously multifarious with a variety of symptoms that include, but are not limited to:
- Repeated instances of joint and ligament injuries such as sprains and dislocations;
- Stiffness in the joints and muscles;
- Pronounced tiredness;
- Impaired equilibrium or clumsiness;
- Disturbances in bowel and bladder functions;
- Joints emitting clicking sounds;
- Easily bruising skin;
- Episodes of dizziness and fainting;
- Scars that are abnormal in appearance;
- Skin that is unusually thin and stretchy.
JHS impacts every individual differently, thus the severity and range of symptoms can vary significantly. This highlights the importance of understanding these symptoms for early detection and more effective management of this syndrome.
Diving Deep into Joint Hypermobility Syndrome: Causes, Risk Factors, and the Role of Collagen
Joint Hypermobility Syndrome (JHS) is an intriguing and complex connective tissue disorder whose root cause remains elusive. Despite this, several correlations and hypotheses exist to shed some light on its origin and its relationship to one’s genetics and collagen formation.
The Genetic Connection and Collagen in JHS
Although the exact cause of JHS remains shrouded in mystery, a significant correlation has been noted between the appearance of JHS and an individual’s genetic lineage. Families with a history of the condition suggest the possibility of a genetic predisposition towards developing JHS.
A central player within this theoretical framework is collagen. This protein, often called the ‘body’s scaffolding,’ is responsible for maintaining the skin, joints, ligaments, and tendons’ integrity and elasticity. It’s hypothesized that individuals with JHS have collagen that is subpar in strength and over-flexible, leading to the characteristic manifestation of overly flexible joints associated with this syndrome.
This collagen malfunction is believed to stem from a defect in the genetic blueprint responsible for its production, leading to structurally flawed collagen molecules.
Factors Influencing the Emergence of Joint Hypermobility Syndrome
While heredity appears to play a significant role in JHS’s emergence, various other factors can influence its onset:
- Muscle Tone: Low muscle tone or hypotonicity can contribute to a wider range of joint movements, increasing hypermobility;
- Gender Correlation: JHS tends to be more prevalent among women compared to men;
- Aging Effect: With age, the collagen fibers in ligaments naturally bind more securely, reducing flexibility. This can make previously hypermobile and pain-free individuals, less flexible as they approach their middle ages;
- Ethnicity: Certain ethnicities, specifically individuals of Asian or West African descent, show a higher prevalence of JHS;
- Neurological conditions: Research has revealed a higher tendency for people with neurological conditions like autism, ADHD, and Tourette’s syndrome to exhibit symptoms of JHS.
Deciphering Joint Hypermobility Syndrome: Diagnostic Approaches and Tools
The identification of Joint Hypermobility Syndrome (JHS) revolves around a combination of physical examinations and certain tests designed to assess joint flexibility and mobility. It’s also critical to rule out other potential genetic conditions that can mimic similar symptoms.
Unveiling JHS: The Beighton Score System
Fundamental in diagnosing JHS is the utilization of a scoring system known as the Beighton Score. This system evaluates joint flexibility across a nine-point scale, assigning one point for successful completion of each of the following movements:
- Touching the ground with flat hands while keeping the knees straight (1 point);
- Bending the elbows in a reverse direction (1 point per elbow);
- Bending the knees backward (1 point per knee);
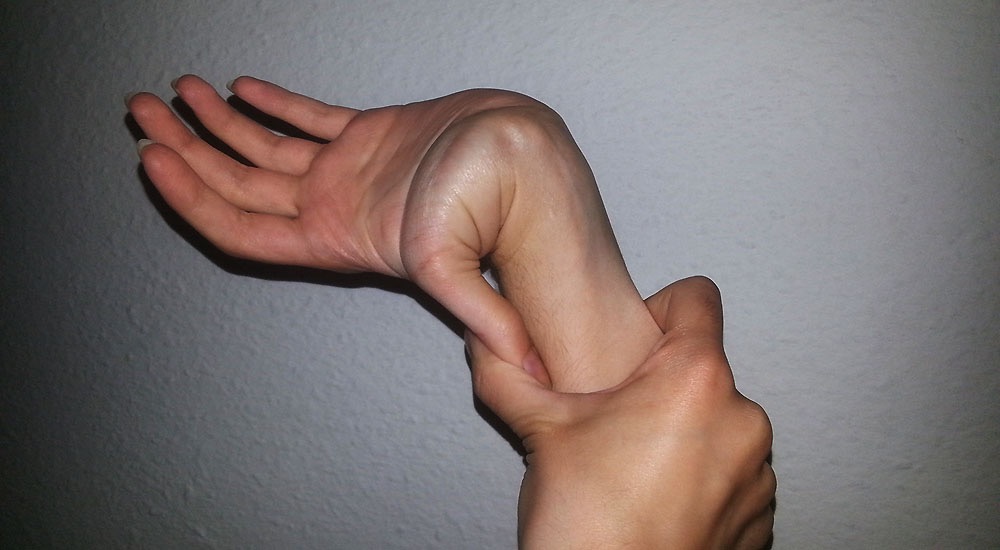
- Touching the forearm with the thumb by pulling it backward (1 point per thumb);
- Bending the little finger backward beyond 90 degrees (1 point per side).
Age-Related Changes and the Need for Historical Assessment
The progression of age naturally brings about a decrease in joint mobility. This known fact necessitates asking questions related to your past joint flexibility. Here are some key questions:
- Have you ever been able (or can you still) touch the ground with hands flat while keeping the knees unbent?;
- Could you ever (or can you still) bend your thumb to reach your forearm?;
- Were you known for your ability to perform unusual body contortions or the splits as a child?;
- Have you ever experienced more than one dislocation of your shoulder or kneecap during childhood or your teenage years?
Answering “yes” to a couple or more of these questions may raise suspicions of JHS.
Managing Joint Hypermobility Syndrome: Tools, Techniques, and Lifestyle Modifications
While Joint Hypermobility Syndrome (JHS) is a hereditary condition, the associated symptoms and impacts on daily life can be effectively managed with the right knowledge, tools, and techniques. Working in collaboration with an experienced podiatrist is pivotal in developing a customised plan to alleviate symptoms and protect the joints.
Bolstering Physical Wellness
Implementing certain exercises and physical strategies can go a long way in enhancing joint stability and reducing discomfort:
- Educate yourself on the most suitable exercises that can strengthen your joints without causing harm or overextension;
- Focus on specific muscle-strengthening exercises to enhance overall balance and stabilise joints;
- Consider employing methods like muscular taping or braces to improve gait and prevent injuries;
- Utilise ergonomic footwear or modified shoes along with personalised orthotics;
- Participate in a customised exercise regimen formulated according to your unique needs;
- Incorporate regular exercise sessions interspersed with ample rest periods into your daily routine.
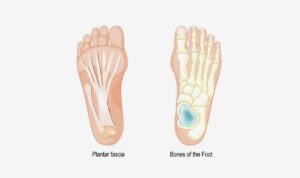
Addressing Foot Shape Variations
Individuals with JHS often exhibit a wide range of foot shapes. While flat feet are common, some may have high arches. Both types can cause pain and impact walking abilities. Moreover, these individuals present a heightened risk of strains, sprains, dislocations besides higher instances of osteoporosis.
To manage these issues, a podiatrist can comprehensively assess joint strength, gait, conduct function tests, and introduce braces or custom-made foot orthotics. These serve to uphold the feet and legs, decrease harmful movements and prevent injury.
Types of braces such as the Exo-Brace and the Richie brace can curb ankle instability and foot drop, thereby reducing foot pain and subsequent problems.
Conclusion
In conclusion, Joint Hypermobility Syndrome presents unique challenges for individuals experiencing increased joint flexibility and associated symptoms, including the need for comprehensive care such as fungal nail treatment. Understanding the causes, symptoms, risk factors, and treatment options for this condition is essential for effective management and improved quality of life. Collaborating with healthcare professionals, staying proactive in symptom management, and adopting lifestyle modifications can empower individuals with Joint Hypermobility Syndrome to lead fulfilling lives while minimizing the impact of hypermobility-related complications, including those necessitating fungal nail treatment. By raising awareness and promoting early intervention, we can enhance outcomes for individuals living with Joint Hypermobility Syndrome and pave the way for a healthier, more resilient future.