Key Questions of this article:
- What Exactly Are Shin Splints?;
- Can Shin Splints Affect Both Legs at the Same Time?;
- What Activities Are Most Likely to Cause Shin Splints?;
- How Can I Prevent Shin Splints?;
- What Should I Do If I Think I Have Shin Splints?
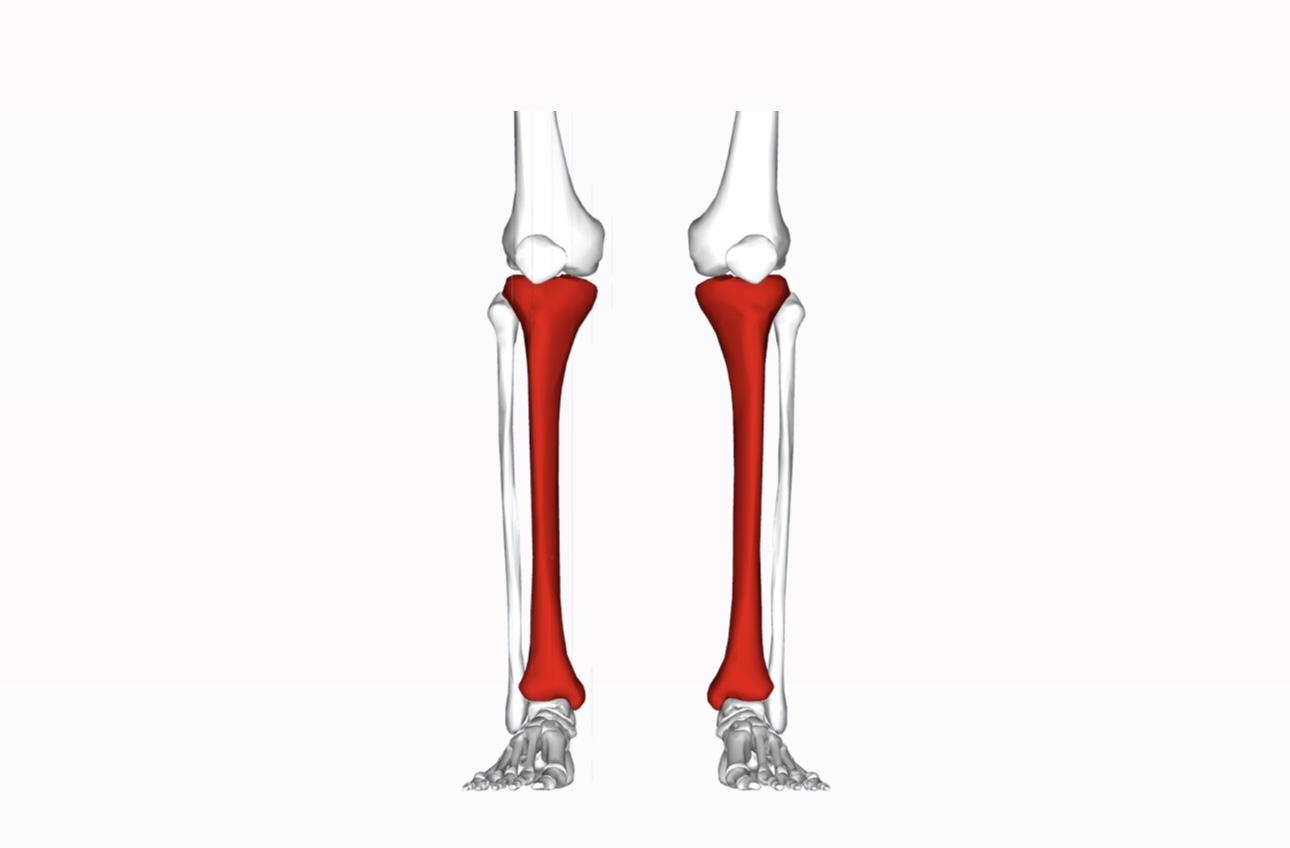
Individuals who feel pain along their lower legs, particularly on the shin bone, might be dealing with medial tibial stress syndrome, which is more widely recognized as shin splints. This condition emerges when the muscles, tendons, and tissues surrounding the shin bone, or even the bone itself, suffer from inflammation or swelling. Such a scenario typically arises from overuse and repetitive stress that overwhelms the area, rendering it incapable of proper recovery amidst continual high stress and activity levels. Shin splints, a prevalent affliction, can impact either one or both lower legs, manifesting as pain, stiffness, and swelling along the inner edge of the shin bone.
Causes & Risk Factors
The principal cause of shin splints is identified as the overuse stemming from exercise and daily activities. This overuse leads to a perpetual state of fatigue in the shin bone and surrounding soft tissue structures, diminishing their capacity to absorb excessive shock forces. Individuals engaged in physical activities, especially those involving weight-bearing or running-based sports such as AFL, basketball, dancing, netball, and soccer, are at an elevated risk. The swift stops, starts, and direction changes characteristic of these sports exert additional strain on the leg muscles and tendons, hastening fatigue. Factors contributing to shin splints also encompass:
- Commencing intense training without a gradual increase in load;
- Inadequate warm-up routines;
- Running or jumping on hard or uneven surfaces;
- Utilizing unsuitable or worn-out footwear;
- Lower limb strength, mobility, and flexibility deficits;
- Rigid, inflexible feet poorly equipped for shock absorption;
- Muscle imbalances and dysfunctions;
- Flat feet or high arches;
- Excessive inward rolling of the foot (overpronation);
- Differences in leg length;
- Bowed or knocked knees;
- Abnormal walking and running patterns.
Symptoms
The hallmark of shin splints is pain along the inside of the lower leg, adjacent to the shin bone. Initially, this pain may intensify at the beginning and end of exercise sessions but might subside during the activity. As the condition progresses, pain could persist during both activity and rest. Additional symptoms include mild swelling, tenderness, and a dull, aching sensation. Given the similarity of shin splint symptoms to other conditions, a proper diagnosis from a podiatrist is crucial to ensure appropriate treatment.
Diagnosis
The similarity of shin splint symptoms to those of tendonitis necessitates accurate diagnosis by podiatrists. This involves reviewing current symptoms, conducting a physical assessment of the lower limbs, and possibly employing diagnostic imaging to detect stress fractures or reactions.
Treatment
Prompt initiation of treatment is vital to prevent the progression to stress fractures and facilitate swift recovery. Addressing the underlying causes is the first step, followed by a tailored combination of treatments for optimal recovery. This regimen may include rest, ice, compression, and elevation (RICE) for temporary pain relief, alongside strengthening, stretching exercises, foot mobilisation techniques, adjustments to training programs, supportive footwear, custom orthotics, foot and ankle strapping, shockwave therapy, dry needling, and gait retraining. A cautious return to exercise, with a gradual increase in intensity, is essential to avoid recurrence.
Potential Consequences of Ignoring Shin Splints
Neglecting medial tibial stress syndrome may lead to stress fractures in the shin bones, potentially necessitating the use of a moon boot for an extended duration or even crutches.
Prevention
Preventative measures against shin splints include proactive changes in lifestyle and physical activity routines, such as seeking advice on appropriate footwear, having movement patterns analyzed by a podiatrist, warming up and stretching before sports or exercise, gradually increasing training intensity, and regularly performing podiatrist-recommended lower leg strengthening and conditioning exercises.
Conclusion
In conclusion, shin splints, or medial tibial stress syndrome, represent a significant challenge for individuals engaged in physical activities, especially those involving repetitive stress and impact on the lower legs. Understanding the causes and risk factors, such as overuse, inadequate footwear, and improper training practices, is crucial for both prevention and effective management of this condition. Recognizing the symptoms early on and seeking professional diagnosis and treatment can prevent the progression to more severe injuries like stress fractures. Implementing a comprehensive treatment plan that includes rest, appropriate exercises, and possibly adjustments in footwear and activity patterns, is essential for recovery. Moreover, adopting preventive strategies, including proper warm-up routines, gradual training intensification, and attention to footwear, can significantly reduce the risk of shin splints. By prioritizing lower leg health and adhering to recommended practices, individuals can continue to enjoy physical activities while minimizing the risk of injury. This balanced approach underscores the importance of proactive care, early intervention, and a commitment to maintaining overall musculoskeletal health to combat the onset and recurrence of shin splints.
FAQs:
Shin splints, medically known as medial tibial stress syndrome, occur when the muscles, tendons, and bone tissue around the shin bone (tibia) become inflamed. This condition is often the result of repetitive stress and overuse, leading to pain, stiffness, and swelling along the inner side of the shin.
Yes, shin splints can affect one or both lower legs. The severity of symptoms, including pain and swelling, can vary from one leg to the other. Activities that place a similar level of stress on both legs, like running or dancing, often lead to bilateral shin splints. It’s crucial to understand that the condition stems from overuse or increased stress on the shinbone and its surrounding tissues. Factors contributing to bilateral shin splints include improper footwear, sudden increases in physical activity, or running on hard surfaces. Early detection and treatment are key to preventing chronic issues. Rest, ice, and appropriate exercises can help alleviate symptoms and address the underlying causes. Consulting with a healthcare professional for a personalized treatment plan is advisable for those experiencing persistent or severe symptoms.
Shin splints are commonly associated with activities that involve repetitive leg impact, such as running, dancing, and sports that require quick stops and starts or direction changes. These activities put a significant load on the shin bone and surrounding tissues, leading to the condition. The repetitive nature of these movements, especially on hard surfaces or without proper footwear, significantly increases the risk. Athletes, dancers, and military recruits are particularly susceptible due to the intense physical demands of their training routines. Prevention strategies include gradually increasing the intensity of activities, using proper footwear, and incorporating strength training and flexibility exercises to improve leg muscle balance and alignment. Recognizing early symptoms and modifying activities can prevent the progression to more severe pain or injury.
Preventing shin splints involves several strategies: wearing appropriate footwear, gradually increasing the intensity of physical activities, warming up properly before exercise, and engaging in exercises that strengthen and condition the lower leg muscles. Additionally, assessing and correcting biomechanical issues with a podiatrist’s help can further reduce the risk.
If you suspect you have shin splints, the first step is to reduce or modify your physical activity to alleviate stress on your shins. Applying ice, rest, and over-the-counter pain relievers can help manage pain and swelling. It’s also important to consult with a healthcare professional, such as a podiatrist, for a proper diagnosis and treatment plan. Ignoring the symptoms can lead to more serious injuries, such as stress fractures.