The post Ingrown Toenails: Antibiotics Aren’t the Answer appeared first on PodiAtry NZ.
]]>Key questions
Questions Addressed:
- What are the underlying causes of ingrown toenails?;
- What physiological processes occur below the surface of an ingrown toenail?;
- What are the potential risks and complications associated with untreated ingrown toenails?;
- How can individuals effectively manage and prevent ingrown toenails?;
- Why is proper foot care essential in addressing ingrown toenails?
What antibiotics treat ingrown toenails?
When it comes to treating ingrown toenails, antibiotics aren’t usually the first line of defense. However, if an ingrown toenail gets infected, antibiotics can help clear up the infection.
Remember, while antibiotics can tackle infections, they won’t fix the ingrown nail itself. For that, we’ll need to remove the ingrown part of the nail, either with simple methods or minor surgery. So, if you’re dealing with an ingrown toenail, don’t hesitate to reach out – we’re here to help you get back on your feet!
What’s Going On Below The Surface Of An Ingrown Toenail?
Ingrowing toenails occur when the edge of your toenail grows into the surrounding skin instead of growing straight out. This can happen due to factors such as improper nail trimming, wearing tight shoes, injury, or naturally curved toenails.
Underneath the surface of an ingrown toenail, you can experience inflammation, redness, and pain as the toenail presses into the soft tissues. The skin around the ingrown toenail may become swollen and tender. Sometimes this can lead to infection, which is characterized by increased pain, warmth, pus, and possibly an unpleasant odor.
Left untreated, an ingrown toenail can worsen and lead to more serious problems like abscesses or even systemic infection. Treatment usually involves soaking your foot in warm, soapy water to soften the skin, gently lifting the edge of the toenail, and occasionally using antibiotics or considering surgery, especially if there’s an infection or the problem persists.
What Will Fix My Ingrown Toenail?
Do you have an ingrown toenail? Don’t worry, it’s a common problem and we have some simple solutions. Start by soaking your foot in warm, soapy water to relieve discomfort and reduce swelling. Then use a clean cotton ball or piece of dental floss to gently lift the edge of the ingrown nail away from the skin.
Here’s the key: Let the pros do the cutting. If it’s a mild case, we can gently trim the nail to relieve the pressure. More serious conditions, however, may require us to remove part of the nail or do a minor procedure to permanently fix the problem.
The bottom line is that if you’re bothered by an ingrown toenail, we have the tools and the know-how. We’ve got the tools and know-how to get your toe back to normal in no time.
Permanent Ingrown Toenail Removal Options
When it comes to dealing with pesky ingrown toenails for good, there are a few options to consider:
- Partial Nail Avulsion: This procedure involves removing a portion of the nail border where the ingrown nail is causing trouble. It’s a relatively simple and effective solution, often performed under local anesthesia in a doctor’s office;
- Total Nail Avulsion: In more severe cases or for recurrent ingrown toenails, removing the entire nail may be necessary. This allows for a fresh start and prevents the nail from growing back ingrown;
- Chemical Matrixectomy: This involves applying a chemical solution to the nail matrix, the area where the nail grows from, to prevent regrowth of the ingrown portion of the nail. It’s typically reserved for chronic or severe cases.;Surgical Intervention: For persistent or complicated ingrown toenails, surgical procedures such as matrixectomy with nail bed repair or nail bed reconstruction may be recommended. These options involve more extensive surgery and are usually considered when other treatments have failed.
Before deciding on a course of action, it’s essential to consult with a healthcare professional who can assess your specific situation and recommend the most appropriate treatment for you.
Treating Ingrown Nails Effectively Means Understanding Its Cause
To effectively tackle the discomfort of ingrown nails, it’s crucial to grasp their underlying causes. Ingrown nails typically occur when the edges of the toenail grow into the surrounding skin, leading to pain, inflammation, and potential infection. Several factors contribute to this condition:
- Improper Nail Trimming: Cutting nails too short or rounding the edges can encourage them to grow into the skin;
- Poorly Fitting Footwear: Tight shoes or socks can exert pressure on the toes, pushing the nails into the skin;
- Trauma or Injury: Stubbing your toe or repetitive activities that stress the toes can cause ingrown nails;
- Genetic Predisposition: Some individuals may have a genetic predisposition to ingrown nails due to the shape or structure of their nails.
Once the cause is identified, appropriate treatment strategies can be implemented. This may include soaking the foot in warm water, gently lifting the ingrown edge, wearing properly fitting footwear, and seeking professional help for severe cases. By addressing the root cause, we can effectively alleviate discomfort and promote healthy nail growth.
Conclusion
The discomfort and potential complications of ingrown toenails underscore the importance of proper foot care and timely intervention. By recognizing the signs and symptoms early on, individuals can take proactive measures to prevent ingrown toenails from developing or worsening. Whether through diligent nail trimming techniques, wearing properly fitting footwear, or seeking prompt medical attention when needed, addressing ingrown toenails effectively can improve overall foot health and quality of life. Remember, a little attention to your feet can go a long way in avoiding the discomfort and inconvenience of ingrown toenails.
The post Ingrown Toenails: Antibiotics Aren’t the Answer appeared first on PodiAtry NZ.
]]>The post Mastering Lower Leg Pain: Expert Guide & Exercises appeared first on PodiAtry NZ.
]]>Common symptoms of a pulled or strained calf
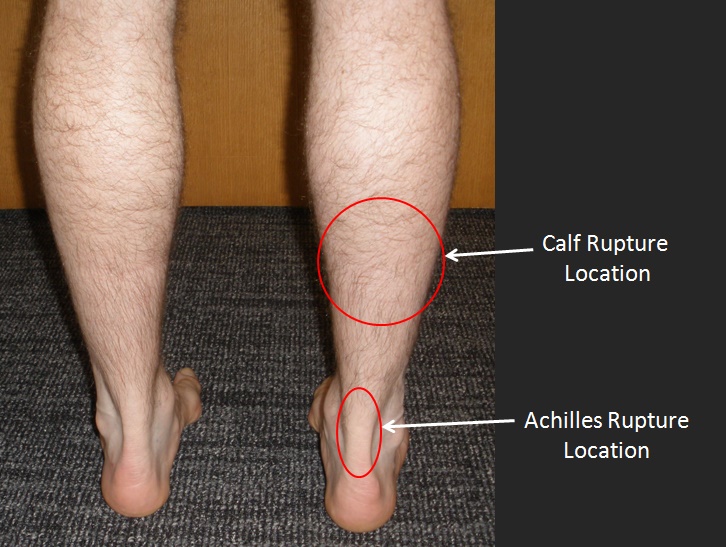
Symptoms of a pulled or strained calf muscle commonly include:
- Pain: You may experience sharp or dull pain in the calf muscle. The pain may range from mild to severe depending on the extent of the injury;
- Swelling: Swelling around the affected area is typical after a calf strain or pull. The swelling may cause the calf to feel tight and tender to the touch;
- Bruising: In some cases, bruising may develop around the calf muscle due to small blood vessel damage resulting from the strain;
- Weakness: The injured calf muscle may feel weak, making it difficult to walk, stand, or bear weight on the affected leg;
- Stiffness: Stiffness in the calf muscle and difficulty moving the ankle or foot may occur after a strain;
- Limited Range of Motion: You may find it challenging to flex or extend your foot and ankle fully due to the pain and stiffness associated with the injury;
- Popping Sensation: Some individuals report hearing or feeling a popping sensation at the time of injury, though this isn’t always present.
If you’re dealing with a strain, remember to give that leg some rest. Ice packs are your best friend for reducing swelling, and it’s a good idea to elevate your leg too. Try to avoid activities that make the pain worse – it’s all about giving your ankle a chance to heal.
Now, if you’re dealing with a severe strain and you notice some serious bruising, if you can’t bear weight on it, or if the pain just won’t quit despite home treatment, it’s time to give us a call. We’re here to help, and sometimes a little extra medical attention is just what the doctor ordered!
Strengthening exercises for lower leg pain
Lower leg pain can arise from various causes such as muscle imbalances, overuse injuries, or underlying conditions like shin splints or tendinitis. Strengthening exercises can help address these issues by improving muscle strength, flexibility, and endurance. Here are some exercises that can help alleviate lower leg pain:
Calf Raises:

- Stand with feet hip-width apart, then rise onto your toes, lifting your heels as high as possible;
- Slowly lower your heels back down;
- Perform 2-3 sets of 10-15 repetitions.
Ankle Dorsiflexion:
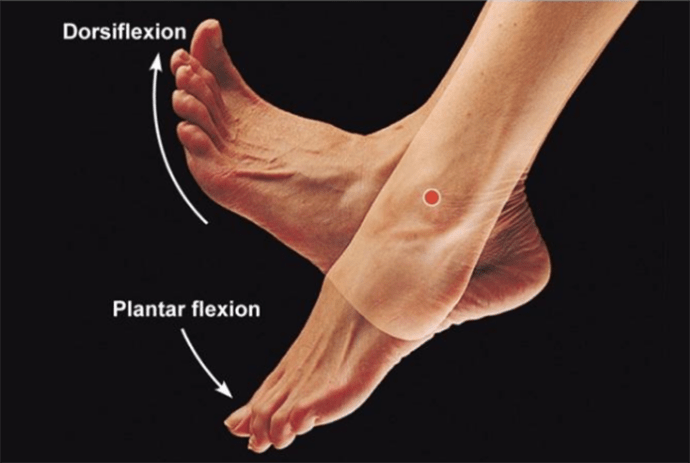
- Sit on a chair with your feet flat on the floor;
- Loop a resistance band around the top of your foot and hold the ends in your hands;
- Flex your ankle upward against the resistance of the band, then slowly return to the starting position;
- Perform 2-3 sets of 10-15 repetitions for each foot.
Ankle Alphabet:
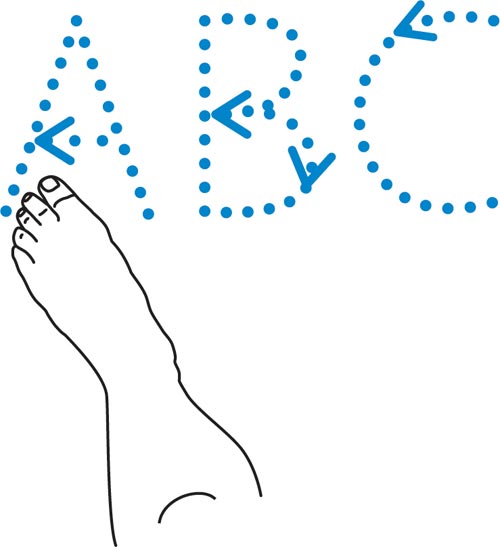
- Sit on a chair with one leg extended;
- Pretend your big toe is a pencil and “write” the alphabet in the air with your foot;
- Perform this exercise with each foot for 2-3 sets.
Towel Scrunches:

- Sit on a chair with both feet flat on the floor;
- Place a small towel on the floor in front of you;
- Use your toes to scrunch up the towel, pulling it toward you;
- Repeat for 2-3 sets of 10-15 repetitions.
Remember to start with light resistance or repetitions and gradually increase as your strength improves. If you experience any pain during these exercises, stop immediately and consult with a healthcare professional. Additionally, it’s essential to combine strengthening exercises with proper rest, stretching, and adequate nutrition for optimal recovery and injury prevention.
Stretching exercises for lower leg pain
Stretching can be beneficial for relieving lower leg pain by improving flexibility, reducing muscle tightness, and enhancing blood circulation. Here are some stretching exercises specifically targeting the lower leg:
Calf Stretch:
- Stand facing a wall with your hands resting on the wall at shoulder height;
- Take a step back with one foot, keeping it straight with the heel flat on the ground;
- Bend your front knee slightly and lean forward, keeping your back leg straight until you feel a stretch in your calf muscle;
- Hold for 20-30 seconds, then switch legs;
- Repeat 2-3 times on each leg.
Gastrocnemius Stretch:
- Sit on the floor with your legs extended straight out in front of you;
- Loop a towel or resistance band around the ball of one foot and gently pull it towards you;
- Keep your knee straight and your heel on the ground until you feel a stretch in the calf of the straightened leg;
- Hold for 20-30 seconds, then switch legs;
- Repeat 2-3 times on each leg.
Soleus Stretch:
- Sit on the floor with one leg extended straight out in front of you and the other leg bent with the foot flat on the floor;
- Lean forward, reaching towards your toes while keeping your back straight;
- You should feel a stretch in the lower part of your calf;
- Hold for 20-30 seconds, then switch legs;
- Repeat 2-3 times on each leg.
Towel Stretch:
- Sit on the floor with your legs extended straight out in front of you;
- Loop a towel around the ball of one foot and hold onto both ends with your hands;
- Gently pull the towel towards you, flexing your foot back towards your body until you feel a stretch in your calf;
- Hold for 20-30 seconds, then switch legs;
- Repeat 2-3 times on each leg.
Ankle Flexion Stretch:
- Sit on the floor with your legs extended straight out in front of you;
- Flex your foot back towards your body, pointing your toes up towards the ceiling;
- Hold onto your toes with your hands and gently pull them towards you until you feel a stretch in your calf and ankle;
- Hold for 20-30 seconds, then relax;
- Repeat 2-3 times.
Tibialis Anterior Stretch:
- Stand facing a wall with your hands resting on the wall at shoulder height;
- Place one foot behind the other and slightly bend both knees;
- Lean forward, keeping your back heel on the ground until you feel a stretch in the front of your shin;
- Hold for 20-30 seconds, then switch legs;
- Repeat 2-3 times on each leg.
Perform these stretching exercises regularly, especially after physical activity or when you experience tightness or discomfort in your lower legs. Avoid bouncing during stretches, and remember to breathe deeply and relax into each stretch for maximum effectiveness. If you have any existing medical conditions or concerns, consult with a healthcare professional before starting a new stretching routine.
Aerobic Exercise for lower leg pain
Engaging in low-impact aerobic exercises can be beneficial for managing lower leg pain by improving circulation, strengthening muscles, and promoting overall fitness without placing excessive strain on the lower limbs. Here are some low-impact aerobic exercises that can help alleviate lower leg pain:
- Walking: Walking is an excellent low-impact exercise that can improve cardiovascular health and strengthen the muscles in your lower legs. Start with short distances and gradually increase your pace and duration as tolerated;
- Cycling: Cycling, whether outdoors or on a stationary bike, is another effective low-impact exercise that can help alleviate lower leg pain. It strengthens the muscles in your legs without putting too much stress on your joints;
- Swimming: Swimming is a full-body workout that provides cardiovascular benefits while being gentle on the joints. It can help improve circulation and strengthen muscles throughout the body, including the lower legs;
- Elliptical Training: Using an elliptical machine provides a low-impact, full-body workout that mimics the motion of walking or running without the jarring impact on the lower limbs. It can help improve cardiovascular fitness and strengthen the muscles of the lower legs;
- Water Aerobics: Participating in water aerobics classes or exercises in a pool can provide a low-impact cardiovascular workout while also providing resistance from the water to strengthen muscles. Water buoyancy reduces the stress on the lower limbs;
- Rowing Machine: Rowing is a low-impact, full-body workout that engages the muscles in the legs, arms, and core. It can improve cardiovascular fitness and muscle strength without putting excessive strain on the lower legs;
- Tai Chi: Tai Chi is a gentle form of martial arts that involves slow, flowing movements and deep breathing. It can help improve balance, flexibility, and muscle strength, which may help alleviate lower leg pain.
When engaging in aerobic exercise to alleviate lower leg pain, it’s essential to start gradually and listen to your body. If you experience increased pain or discomfort, stop the activity and consult with a healthcare professional. Additionally, consider incorporating stretching and strengthening exercises specific to the lower legs to further support pain relief and prevent future issues.
Conclusions
Well folks, as we wrap up our chat about Chronic Ankle Instability, let’s keep in mind that knowledge is key. By staying informed and taking action, we can tackle this condition head-on with confidence and hope. Together, let’s journey towards a brighter, more comfortable future for your ankles and your overall quality of life!
The post Mastering Lower Leg Pain: Expert Guide & Exercises appeared first on PodiAtry NZ.
]]>The post Unraveling Chronic Ankle Instability: In-Depth Exploration appeared first on PodiAtry NZ.
]]>As we embark on a journey to unravel the intricacies of Chronic Ankle Instability, we delve into its origins, symptoms, diagnostic approaches, and diverse treatment modalities. Through this exploration, we aim not only to illuminate the path toward understanding but also to offer hope and empowerment to those grappling with this debilitating condition.
Key questions
Questions Addressed:
- What defines Chronic Ankle Instability?;
- What are the symptoms and implications of Chronic Ankle Instability?;
- What factors contribute to the development of Chronic Ankle Instability?;
- How is Chronic Ankle Instability diagnosed?;
- What treatment options are available for Chronic Ankle Instability?;
- How can Chronic Ankle Instability be prevented?;
- What are the broader implications of Chronic Ankle Instability on daily life and mobility?
What Is Chronic Ankle Instability?
Chronic ankle instability (CAI) refers to a condition characterized by recurrent ankle sprains, feelings of giving way or instability, and persistent discomfort or pain in the ankle joint. It typically arises after an initial ankle sprain that does not fully heal or properly rehabilitate, leading to ongoing issues with the stability of the ankle joint.
CAI can result from various factors, including inadequate rehabilitation following an ankle sprain, ligament laxity, structural abnormalities in the ankle joint, weakness in the muscles surrounding the ankle, and proprioceptive deficits (problems with the body’s awareness of its position in space). Individuals with CAI often experience episodes of the ankle “giving way” or feeling unstable during activities that involve walking, running, or jumping.
Management of chronic ankle instability typically involves a combination of interventions, including physical therapy to strengthen muscles and improve proprioception, bracing or taping to provide external support to the ankle, activity modification to avoid aggravating movements, and sometimes surgical intervention in severe cases. The goal of treatment is to improve ankle stability, reduce the risk of recurrent sprains, and alleviate associated symptoms.
Signs & Symptoms Of Chronic Ankle Instability

Chronic ankle instability (CAI) can manifest through various signs and symptoms, which may include:
- Recurrent ankle sprains: Individuals with CAI often experience repeated ankle sprains, even with minimal force or movement;
- Feeling of ankle giving way: A common complaint among individuals with CAI is a sensation that the ankle is giving way or unstable, particularly during weight-bearing activities like walking, running, or jumping;
- Persistent discomfort or pain: Chronic pain or discomfort in the ankle joint, which may vary in intensity and can be present both during activity and at rest;
- Swelling: Swelling around the ankle joint may occur, particularly following episodes of instability or injury;
- Difficulty with balance: Instability in the ankle joint can lead to difficulties with balance and coordination, especially on uneven surfaces or during activities that require precise foot placement;
- Weakness in the ankle: Muscular weakness, particularly in the muscles that support and stabilize the ankle, may be present in individuals with CAI;
- Limited range of motion: Reduced flexibility and range of motion in the ankle joint, which can contribute to feelings of instability and difficulty with certain movements;
- Pain with certain movements: Pain or discomfort may be elicited with specific movements of the ankle, such as dorsiflexion (bringing the foot upwards) or inversion/eversion (rolling the foot inward or outward);
- Stiffness: Some individuals with CAI may experience stiffness in the ankle joint, particularly following periods of inactivity or after waking up in the morning;
- Functional limitations: CAI can lead to functional limitations in daily activities, sports participation, and other physical tasks due to the fear of reinjury or exacerbating symptoms.
It’s essential for individuals experiencing these signs and symptoms to seek evaluation and appropriate management from a healthcare professional, such as a physician or physical therapist, to prevent further complications and improve ankle stability.
What Causes Chronic Ankle Instability?
Chronic ankle instability (CAI) can result from a combination of factors, including acute ankle injuries that are not adequately treated or rehabilitated, anatomical abnormalities, and neuromuscular deficits. Some common causes and contributing factors include:
- Acute ankle sprains: An initial ankle sprain can weaken the ligaments and surrounding structures of the ankle, leading to instability over time if not properly rehabilitated;
- Incomplete healing: Failure to fully heal from an ankle sprain or returning to activity too soon after an injury can result in lingering instability;
- Ligament laxity: Some individuals naturally have looser ligaments, making them more prone to ankle sprains and instability;
- Muscle weakness: Weakness or imbalance in the muscles surrounding the ankle, particularly the peroneal muscles on the outer aspect of the ankle, can contribute to instability;
- Proprioceptive deficits: Proprioception refers to the body’s ability to sense its position in space. Ankle injuries can disrupt proprioceptive feedback, leading to decreased coordination and balance, which can contribute to instability;
- Anatomical factors: Structural abnormalities in the ankle joint, such as a high arch or flat foot, can increase the risk of ankle instability;
- Previous injuries: Individuals who have experienced multiple ankle injuries or have a history of ankle instability are more likely to develop chronic ankle instability;
- Poor footwear: Inappropriate footwear or inadequate ankle support during physical activity can increase the risk of ankle injuries and instability;
- Environmental factors: Participating in activities that involve uneven surfaces, sudden changes in direction, or high-impact movements can increase the risk of ankle injuries and contribute to chronic instability;
- Genetic predisposition: Some individuals may have a genetic predisposition to ankle instability, making them more susceptible to recurrent sprains and chronic instability.
Overall, chronic ankle instability is often multifactorial, with a combination of anatomical, biomechanical, and neuromuscular factors contributing to its development. Effective management typically involves addressing these underlying factors through rehabilitation, strengthening exercises, proprioceptive training, bracing or taping, and sometimes surgical intervention in severe cases.
How To Diagnose Chronic Ankle Instability

Diagnosing chronic ankle instability (CAI) typically involves a comprehensive evaluation by a healthcare professional, such as a physician or a physical therapist. The diagnostic process may include the following steps:
- Medical history: The healthcare provider will inquire about the patient’s medical history, including any previous ankle injuries, the frequency and severity of symptoms, and any treatments or interventions that have been attempted;
- Physical examination: A thorough physical examination of the ankle joint will be conducted to assess for signs of instability, such as laxity of the ligaments, swelling, tenderness, and range of motion deficits. Special tests, such as the anterior drawer test and talar tilt test, may be performed to assess ligament stability;
- Functional assessment: The healthcare provider may assess the patient’s functional abilities, balance, and proprioception through various functional tests and maneuvers. This helps to determine the impact of ankle instability on daily activities and sports participation;
- Imaging studies: In some cases, imaging studies such as X-rays, MRI (magnetic resonance imaging), or CT (computed tomography) scans may be ordered to assess the extent of ligament damage, evaluate for structural abnormalities, and rule out other potential causes of ankle pain and instability, such as fractures or osteochondral lesions;
- Gait analysis: Observing the patient’s gait pattern and walking mechanics can provide valuable information about any abnormalities or compensatory movements that may contribute to ankle instability;
- Functional testing: Functional tests, such as single-leg balance tests, hopping tests, and agility drills, may be performed to assess the patient’s dynamic stability and functional capacity;
- Patient-reported outcome measures: Questionnaires and scales may be used to assess the patient’s symptoms, functional limitations, and quality of life related to ankle instability.
Based on the findings of the evaluation, the healthcare provider can make a diagnosis of chronic ankle instability and develop an appropriate treatment plan. Treatment typically involves a combination of conservative measures, such as physical therapy, bracing or taping, activity modification, and in some cases, surgical intervention to stabilize the ankle joint. Early and accurate diagnosis is crucial for effectively managing chronic ankle instability and preventing further complications.
Treatment For Chronic Ankle Instability

The treatment for chronic ankle instability (CAI) typically involves a combination of conservative measures and, in some cases, surgical intervention. The specific approach to treatment may vary depending on the severity of symptoms, functional limitations, underlying causes, and individual patient factors. Here are some common treatment options:
- Physical therapy: A structured physical therapy program is often the cornerstone of treatment for CAI. Physical therapists can design a customized rehabilitation program aimed at improving ankle strength, flexibility, proprioception, and balance. Exercises may include strengthening exercises for the muscles surrounding the ankle, balance training, and neuromuscular re-education;
- Bracing or taping: External support, such as ankle braces or athletic tape, may be used to provide stability to the ankle joint during physical activity. These devices can help reduce the risk of recurrent sprains and improve proprioceptive feedback. A healthcare provider can recommend the most appropriate type of brace or taping technique based on the individual’s needs and activity level;
- Activity modification: Modifying activities that exacerbate symptoms or increase the risk of ankle injury can help prevent further instability and promote healing. This may involve avoiding high-impact activities, minimizing activities on uneven surfaces, and gradually reintroducing physical activity as symptoms improve;
- Footwear modification: Wearing supportive and properly fitting footwear can help reduce stress on the ankle joint and provide additional stability. Orthotic inserts or custom-made orthotics may be recommended to address underlying biomechanical issues, such as overpronation or supination;
- Proprioceptive training: Proprioceptive exercises aim to improve the body’s awareness of joint position and movement, which is often impaired in individuals with CAI. These exercises may include balance drills, proprioceptive challenges on unstable surfaces, and agility training to enhance neuromuscular control;
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Over-the-counter or prescription NSAIDs, such as ibuprofen or naproxen, may be used to help alleviate pain and inflammation associated with CAI. It’s important to use these medications as directed and under the guidance of a healthcare provider;
- Corticosteroid injections: In some cases, corticosteroid injections may be considered to reduce inflammation and pain in the ankle joint, particularly if symptoms are severe and not responsive to other treatments. However, the use of corticosteroid injections is typically limited due to potential side effects and the risk of weakening the ligaments;
- Surgical intervention: In cases of severe or refractory CAI, surgical intervention may be necessary to restore stability to the ankle joint. Surgical procedures may involve repairing or reconstructing damaged ligaments, addressing structural abnormalities, or stabilizing the joint through arthroscopy or open surgery.
The choice of treatment approach depends on various factors, including the patient’s symptoms, functional limitations, activity level, and response to conservative measures. A healthcare provider, such as an orthopedic surgeon or physical therapist, can help guide treatment decisions and develop an individualized plan to address chronic ankle instability effectively.
Prevention
Preventing chronic ankle instability (CAI) involves addressing risk factors and implementing strategies to reduce the likelihood of ankle injuries. Here are some preventive measures individuals can take:
- Proper rehabilitation: Ensure thorough rehabilitation following an ankle injury, including appropriate rest, immobilization if necessary, and a structured physical therapy program to restore strength, flexibility, and proprioception;
- Ankle strengthening exercises: Incorporate exercises that target the muscles surrounding the ankle, such as calf raises, ankle dorsiflexion and plantarflexion exercises, and ankle eversion and inversion exercises, to improve ankle stability and reduce the risk of future injuries;
- Balance and proprioception training: Perform balance and proprioceptive exercises regularly to enhance joint awareness and neuromuscular control. This can include single-leg balance drills, standing on unstable surfaces (e.g., balance boards or foam pads), and agility drills;
- Footwear selection: Wear supportive and properly fitting footwear that provides adequate cushioning, stability, and traction, especially during physical activity. Consider using orthotic inserts or custom-made orthotics to address biomechanical issues and reduce the risk of overpronation or supination;
- Bracing or taping: Use ankle braces or athletic tape during sports or activities that involve high-risk movements to provide additional support and stability to the ankle joint. A healthcare provider can recommend the most suitable type of brace or taping technique based on individual needs and activity level;
- Gradual return to activity: Gradually reintroduce physical activity and sports participation following an ankle injury, starting with low-impact activities and gradually progressing to higher-intensity exercises. Avoid returning to full activity too soon to allow adequate time for healing and rehabilitation;
- Warm-up and cool-down: Always warm up before engaging in physical activity to prepare the muscles and joints for movement, and cool down afterward to aid in recovery and reduce muscle soreness. Incorporate dynamic stretches and mobility exercises targeting the ankles into your warm-up and cool-down routines;
- Environmental awareness: Be mindful of the surfaces and environments in which you engage in physical activity, avoiding uneven or unstable surfaces whenever possible to reduce the risk of ankle sprains and instability;
- Maintain a healthy weight: Excess body weight can increase stress on the ankles and other joints, potentially predisposing them to injury. Maintaining a healthy weight through regular exercise and a balanced diet can help reduce the risk of ankle injuries;
- Regular assessment and maintenance: Regularly assess your ankle health and functional abilities, and address any issues promptly with appropriate treatment or preventive measures. This may include periodic check-ups with a healthcare provider, ongoing physical therapy, and adjustments to footwear or orthotic devices as needed.
By incorporating these preventive strategies into your routine, you can reduce the risk of developing chronic ankle instability and maintain optimal ankle health for long-term mobility and function.
Conclusions
Chronic Ankle Instability emerges not merely as a physical ailment but as a profound disruptor of daily life, casting a shadow of uncertainty and restriction over even the simplest of movements. Yet, within the depths of this challenge lie opportunities for resilience, empowerment, and healing. By embracing a multidimensional approach encompassing proper diagnosis, tailored interventions, and proactive prevention strategies, individuals can reclaim control over their mobility and well-being.
As we navigate the complexities of Chronic Ankle Instability, let us not falter in our pursuit of solutions, but rather, let us draw strength from our collective efforts to overcome, adapt, and thrive in the face of adversity.
The post Unraveling Chronic Ankle Instability: In-Depth Exploration appeared first on PodiAtry NZ.
]]>The post Ankle Instability: Exercises & Therapeutic Care appeared first on PodiAtry NZ.
]]>- What is ankle instability, and what are the common symptoms and indicators of this condition?;
- Why is proper rehabilitation crucial for the treatment of ankle sprains?;
- What are some guided exercises and regimens that can help improve ankle stability?;
- How do flexibility routines enhance ankle stability, and what specific exercises are recommended?;
- What role does aerobic training play in the rehabilitation of chronic ankle instability?;
- What are the strategies for enhancing ankle stability and preventing further injuries?;
- How important is it to consistently perform ankle strengthening and rehabilitation exercises?;
- Why should ankle pain be addressed promptly, and how can ignoring it lead to further complications?;
- What are the benefits of utilizing ankle support during physical activities?;
- When is it necessary to seek podiatric care for ankle injuries, and what can a podiatrist offer in terms of treatment?
Ankle instability, a condition often stemming from repeated ankle sprains, manifests through a propensity for the ankle to collapse during movement or regular activities. Characterized by a sensation of the ankle “giving way,” this condition can also present with pain as a secondary symptom. Typically, an unstable ankle may feel uncertain and precarious, heightening the risk of further sprains.
Learning how to fix chronic ankle instability is essential for maintaining foot health and stability. In a similar vein, addressing curled toes is also crucial for preventing discomfort and maintaining proper gait mechanics. You may also like to explore strategies for managing curled toes to ensure comprehensive foot care.
The Importance of Proper Rehabilitation for Ankle Sprains
An ankle sprain is the result of the joint being forced into an unnatural position, which can stretch or tear the connective ligaments. Such injuries can impair both the reflexes and strength of the affected joint. Without adequate rehabilitation, these deficits may lead to persistent instability.
Neglected sprains, where the ligaments heal improperly due to inadequate treatment, are a common precursor to ongoing ankle instability. Inadequately rehabilitated sprains can also lead to scar tissue accumulation, contributing to joint stiffness and chronic issues. Thus, it’s crucial to address ankle sprains with proper care and rehabilitation.
While acute ankle instability refers to a recent onset, chronic ankle instability denotes a gradual worsening of the condition over time.
Most instances of chronic instability can be effectively addressed with physical therapy, supportive bracing, and medication. Nonetheless, in extreme cases where conservative treatments fail, surgical intervention may be necessary to repair or rebuild compromised ligaments.
Typical Indicators of Ankle Instability

Individuals experiencing ankle instability might notice various signs, including:
- Sudden inward or outward turning of the ankle;
- An unpredictable ankle that collapses unexpectedly;
- Difficulty supporting weight on the impacted leg;
- Discomfort or persistent pain in the ankle area;
- Sensitivity to touch around the ankle;
- Inflammation or puffiness in the affected ankle.
Guided Regimen for Ankle Stability Improvement
Balanced Single-Leg Hold:
- Position yourself securely behind a chair, using it for support only if necessary;
- Elevate one foot, stabilizing yourself on the foot of the affected ankle;
- Maintain this stance, aiming to prolong the duration incrementally. Start with a ten-second hold on the initial day, increasing by ten seconds daily until a full minute is achieved;
- Perform two additional repetitions to finish a series of three.
Toe-Writing Exercise:
- While seated with both feet on the ground, extend the affected leg forward;
- Using your big toe as a pencil, ‘write’ each letter of the alphabet in the air from A to Z;
- Should discomfort arise, cease the activity; otherwise, complete 2-3 additional sequences.
Elevated Calf Strengthening:
- Locate a raised surface that allows your heels to drop below your toes and have a stable object within reach for support;
- Stand on the edge with feet apart at hip width, the front of your feet stable on the surface, heels extending past it;
- Gradually dip your heels below the toes’ level, using the support as needed;
- Pause in the lowered position for 2-3 seconds, then rise to level the feet with the toes;
- Execute ten repetitions for one complete set, rest, and aim for three full sets.
Flexibility Routines for Enhancing Ankle Stability

Foot Arch Pull with Towel:
- Position yourself seated on the floor, legs extended forward;
- Wrap a long towel around the front of both feet, grasping the ends with your hands, spine aligned;
- Gently draw the towel toward you, keeping your knees straight;
- When you feel a stretch through your foot’s arch, hold for 30 seconds;
- Relax and return to the initial posture;
- Perform two additional repetitions of this stretch.
Wall-Assisted Calf Stretch:
- Face a wall, extending your arms to place palms flat against it, keeping arms outstretched;
- Step one foot forward, slightly bending the knee;
- Extend the other foot back, heel grounded, leg straight;
- Feel the stretch in your calf muscle, maintaining for 30 seconds;
- Step back to the initial position;
- Complete two more repetitions of this stretch.
Ankle Mobility Rotation:
- Position a towel roll or foam roller on the floor;
- Sit with one leg extended, the other knee bent, and position the extended leg’s heel on the roller;
- Rotate your ankle in a clockwise direction for ten rotations;
- Switch direction, rotating your ankle anticlockwise for another ten rotations;
- Switch to the opposite leg and repeat;
- Do two more sets of rotations for each ankle.
Aerobic Training for Chronic Ankle Instability Rehabilitation
Incorporating aerobic exercise into rehabilitation regimens for chronic ankle instability can offer multifaceted benefits, aiding in both recovery and long-term management. These exercises not only target the ankle but also contribute to overall fitness and resilience. Nevertheless, it’s imperative to consult a healthcare provider to tailor the exercise regimen to your individual needs and ensure optimal outcomes.
Usually, a podiatrist, physical therapist, or doctor will suggest a low-impact exercise for rehab, like swimming or riding a stationary bike.
Strategies for Enhancing Ankle Stability and Avoiding Injuries
Consistently Perform Ankle Strengthening and Rehabilitation Exercises
Recovering from an ankle sprain typically involves a regimen of strengthening, balancing, and stretching exercises prescribed by healthcare professionals. A common misconception is that once the ankle feels better, these exercises are no longer necessary. However, adhering to these exercises beyond immediate recovery is crucial for maintaining ankle mobility and preventing complications such as instability. Continuous engagement in the prescribed rehabilitation exercises ensures long-term health and functionality of the ankle.
Address Ankle Pain Promptly
Ignoring any form of ankle pain can lead to further complications, particularly if the pain is associated with a recent injury. Acute ankle sprains, if left untreated, can result in additional ligament damage, complicating the healing and rehabilitation process and increasing the risk of ankle instability. Immediate consultation with a healthcare provider is essential for anyone experiencing sudden ankle pain due to an injury.
Utilize Ankle Support During Physical Activities
The use of ankle braces is a proactive approach to prevent ankle injuries, especially in high-impact sports that involve quick movements, such as hockey, soccer, and basketball. Ankle support, through braces or taping, provides stability and reduces the likelihood of awkward movements that could lead to sprains. Additionally, using ankle support can condition the body to avoid motions that increase the risk of injury.
Warm Up Adequately Before Engaging in Exercise
Preventing ankle sprains and injuries starts with a proper warm-up routine before any physical activity. Warming up increases muscle temperature and flexibility, reducing the stress on ligaments, tendons, and joints, thereby minimizing the risk of sprains. A warm-up should include light to moderate endurance activities, such as jogging, star jumps, or walking lunges, for 5-10 minutes to prepare the body for exercise and safeguard against ankle instability.
Understanding When to Seek Podiatric Care for Ankle Injuries
Podiatrists specialize in addressing medical issues related to the feet and lower limbs, including ankle instability. If you’re experiencing ankle problems, consulting a podiatrist is crucial for accurate diagnosis and effective treatment. Through a comprehensive physical examination, a podiatrist can confirm the presence of ankle instability and tailor a treatment plan suited to your specific condition. This typically involves a combination of bracing and physical therapy as part of a functional rehabilitation program.
Moreover, podiatrists can assess the severity of ankle instability and determine if surgical intervention is necessary. They conduct additional tests if needed and address any concerns or queries you may have about the proposed treatment.
Conclusion
Chronic ankle instability can impose significant challenges. However, a comprehensive and effective rehabilitation plan that includes not only targeted exercises and stretches but also a balanced diet, appropriate preventive measures, and mental well-being considerations can set you on the path to recovery. Always seek professional help when dealing with ankle injuries to ensure an accurate diagnosis and treatment plan.
The post Ankle Instability: Exercises & Therapeutic Care appeared first on PodiAtry NZ.
]]>The post Curved Toes Demystified: A Comprehensive Guide appeared first on PodiAtry NZ.
]]>- What are curly toes and how are they characterized?;
- What are the root causes that lead to the development of curly toes?;
- How can one identify the signs and symptoms of curly toes?;
- What potential complications can arise if curly toes are left untreated?;
- What comprehensive treatment strategies are available for managing curly toes?;
- What preventative measures can be taken to avoid the development of curly toes?;
- How does proper footwear play a role in both the prevention and management of curly toes?;
- What specific conditions are related to curly toes, such as clinodactyly and toe deformities like hammer, claw, and mallet toes?;
- How effective are non-surgical interventions in treating curly toes, and when is surgical intervention considered?;
- What are the common misconceptions about curly toes, and how does the guide address them?
Discovering curled digits in oneself or a child often leads to questions about the origins of this condition, its potential health implications, and the possibility of it correcting itself without medical intervention.
If you’re dealing with curled toes, a condition that often accompanies chronic ankle instability, you may also like reading about how to fix this issue, providing practical steps towards recovery and enhancing ankle support.
Understanding Curly Toes
When individuals seek consultation for curly toes, they typically present with one of two primary conditions:
- Clinodactyly: This condition leads to one or more toes being abnormally curled, often noticeable from birth. The curvature may become more pronounced as the child begins to move and walk, highlighting the need for early detection and management;
- Toe Deformities: This category encompasses conditions like hammer, claw, and mallet deformities, each defined by the curvature’s specific location. These abnormalities impact various joints, leading to unique shapes and patterns of bending in the affected digit.
The Root Causes of Curly Toes
The underlying reasons for curly toes vary significantly based on the specific type of bending observed. Clinodactyly, for example, arises from uneven growth in bone, with one side of a growth plate developing more than the other, leading to curvature. Furthermore, the contraction of tendons on the foot’s underside can cause bending. Such cases might be inherited, associated with conditions like Down’s Syndrome, or idiopathic, with no clear cause identified.
Various factors contribute to the development of toe deformities, including:
- Footwear: Tight or narrow shoes may force toes into a cramped position, promoting bending and curling. This is particularly concerning for those with bunions or high arches, as reduced toe box space exacerbates the issue;
- Toe Injuries: Past injuries to toes or feet can make curly toes more likely to develop as a secondary condition;
- Genetics: An inherited predisposition to certain foot shapes or structures may increase the risk of toe deformities;
- Arthritis: Conditions like rheumatoid arthritis can lead to joint inflammation and deformities, including in the toes, thus elevating the risk of curly toes;
- Muscle Imbalances: Disproportions in the muscles and tendons that facilitate toe movement may cause the toes to curl, resulting in deformities such as hammertoes;
- Nerve Damage: Neuropathy or nerve damage in the foot can lead to muscle weakness and, consequently, toe deformities;
- Bunions: Deformities in the big or little toe can cause muscle weakness and joint bunching in the forefoot and toes, leading to deformities like mallet, hammer, and claw toes.
Identifying the Signs and Symptoms of Curly Toes
Curly toes, encompassing conditions such as clinodactyly and various toe deformities, present with a range of symptoms that can vary in severity from person to person. With clinodactyly, the condition typically affects the third, fourth, and fifth toes. Individuals might experience pain or discomfort due to the abnormal positioning of the toes, particularly when subjected to pressure from snug footwear. However, not everyone with clinodactyly experiences pain.
Common issues resulting from abnormal toe positioning include the formation of corns and calluses due to constant rubbing or pressure. Blisters can also develop, adding to the discomfort. The toenails are not spared; they may become bruised, thicken, flatten, or alter in shape due to the ongoing stress and pressure.
Toe deformities share similar symptoms, with blisters, corns, calluses, and discomfort being common. Unlike clinodactyly, which is often present from birth, toe deformities usually develop over time. Initially, individuals may have straight, normal-looking toes, which gradually change shape in response to various factors like improper footwear, genetic predisposition, or other underlying conditions.
Potential Complications of Untreated Curly Toes
Leaving curly toes untreated can lead to a series of complications that significantly impact daily life and physical activities. The most prominent issues include persistent pain and discomfort, often exacerbated by recurrent corns and blisters. These conditions not only cause direct discomfort but also contribute to the challenge of securing comfortable and suitable footwear. As a result, individuals may find it increasingly difficult to remain standing for extended periods or to participate in activities that require prolonged foot use, such as hiking or engaging in long walks with friends and family.
Comprehensive Treatment Strategies for Curly Toes
Curly toes can be managed through a variety of strategies, tailored to the individual’s specific conditions such as the extent of toe curvature, symptoms, and root causes. After a thorough evaluation, a personalized treatment plan can be developed, potentially including:
- Supportive Devices: Toe props, separators, and splints may be used to alleviate symptoms like pain due to toes rubbing against each other;
- Footwear Adjustments: Opting for shoes with a broader toe box can provide the necessary comfort and support, preventing further aggravation of symptoms or worsening of the condition;
- Custom Foot Orthotics: These devices are designed to redistribute weight and pressure evenly across the toes, easing pain and hindering further curvature;
- Stretching Routines: Exercises aimed at loosening any tight muscles or tendons in the feet that may be contributing to the toe curvature;
- Foot Mobilization Therapy: This approach focuses on freeing up the joints and surrounding soft tissue to improve joint alignment, supported by case studies showing radiographic evidence of improvement;
- Routine Symptom Management: Regular care for symptoms such as corns and calluses, including debridement and specialized skin care, can prevent worsening of discomfort;
- Surgical Intervention: In cases where curly toes are severe, fixed, and significantly impairing quality of life, surgical options may be considered to correct the deformity and alleviate pain.
It’s important to note that while toe deformities like hammertoes do not self-correct, approximately 25% of children with curly toes due to clinodactyly may see spontaneous improvement by the age of six.
Preventing Curly Toes: Effective Strategies and Tips

Preventing curly toes largely centers around mindful footwear choices, given that improper shoes are a major avoidable cause of this condition. Emphasizing comfort and support in footwear selections can significantly mitigate the risk of developing curly toes. Key recommendations include:
- Opt for Well-Fitting, Supportive Shoes: Choose shoes with ample toe space to prevent constriction and support natural foot movements. Avoid tight, narrow shoes and high heels that can exacerbate toe issues;
- Accurate Foot Measurements: Since shoe sizes can vary by brand and style, ensuring a precise fit is crucial. Have your feet measured professionally and select shoes that accommodate the size and shape of your feet well;
- Allow Room for Toe Movement: Ensure there’s about a centimeter (or half a thumb’s width) of space for your longest toe at the shoe’s end, allowing for slight movement and swelling throughout the day;
- Fit Shoes to the Larger Foot: Most individuals have one foot slightly larger than the other. Shoes should fit comfortably on the larger foot to prevent unnecessary pressure on the toes;
- Consider Timing When Shoe Shopping: Feet tend to swell during the day; thus, shopping for shoes in the evening can help account for this natural expansion, ensuring a comfortable fit throughout the day;
- Select Shoes with Wide Toe Boxes and Resilient Soles: This provides your feet with the room they need to move without constraint, reducing the risk of curly toes;
- Steer Clear of Pointed Shoes: Shoes with a narrow or pointed toe box can compress the toes, leading to or worsening curly toes.
FAQs
In some instances, the curling of toes may be inherited, though not invariably. Some individuals might naturally tend towards this due to unique aspects of foot anatomy, muscle distribution, or alignment, traits possibly received from parents. Conversely, external influences such as ill-fitting footwear, foot injuries, or certain medical conditions can also contribute to their development.
Definitely. Podiatrists are experts in treating foot-related conditions and can offer effective solutions for issues like curly toes.
Correcting curly toes naturally varies with the root cause and how severe they are. A podiatrist might recommend several non-invasive strategies, focusing on loosening up stiff muscles and tendons in your foot, which might be causing the toes to curl.
Conclusion
Understanding and addressing curled digits can be challenging. However, with appropriate knowledge and support from healthcare professionals, such as podiatrists, managing this condition becomes more manageable. Depending on their severity and underlying cause, various treatment methods can be applied, including exercises, foot care routines, and making informed footwear choices. Prevention is paramount, thus selecting suitable shoes is crucial in minimizing the risk of developing this condition.
The post Curved Toes Demystified: A Comprehensive Guide appeared first on PodiAtry NZ.
]]>The post Understanding Capsulitis: Causes & Treatments appeared first on PodiAtry NZ.
]]>- What is capsulitis, and why is it commonly experienced in the joints of the feet, especially the second toe?;
- How does capsulitis affect the body’s joints, and what is the science behind the inflammation of the joint capsule?;
- What are the primary causes and risk factors contributing to the development of capsulitis in individuals?;
- What are the distinctive symptoms that indicate the presence of capsulitis?;
- How is capsulitis diagnosed, and why is it important to consult a podiatrist for an accurate assessment?;
- What are the recommended management and treatment options for effectively dealing with capsulitis?;
- What potential complications can arise from neglecting capsulitis, and how can it affect joint stability and function over time?;
- What is the impact and prevalence of capsulitis on individuals’ daily lives and mobility?;
- What prevention tips can individuals follow to reduce the risk of developing capsulitis?;
- Why is comprehensive care important for individuals suffering from capsulitis, and how can it help prevent future recurrences of the condition?
Understanding Capsulitis
Are you experiencing a sensation akin to walking on a pebble every time you take a step? Or perhaps, the ball of your foot feels as if it is under constant pressure from a hard object? If so, your problem could be capsulitis, a condition our podiatrists frequently encounter. Although capsulitis can strike any joint in the body, it is most prevalent in the second toe.
For those interested in understanding how joint inflammation impacts foot health, such as in the case of capsulitis, you may also find the article on curled toes informative. It explores how changes in foot mechanics due to pain and stiffness can lead to related conditions like curled toes.
The Science Behind Capsulitis
The term ‘capsulitis’ denotes inflammation (‘itis’) of the joint capsule. Each joint in your feet is encapsulated within a protective covering that ensures smooth functioning and proper alignment of the joint. Damage to this capsule results in a painful, swollen joint, often giving the feeling of walking on a small stone. Though commonly seen in feet, capsulitis can affect any part of the body with a joint capsule. Adhesive capsulitis, or frozen shoulder, is a well-known example of capsulitis affecting the upper body.
Causes and Risk Factors of Capsulitis
The root cause of capsulitis, a condition marked by joint pain, is primarily attributed to the excessive stress placed on a joint. This overburdening leads to tissue damage and resultant discomfort. Such stress often stems from faulty foot mechanics or from footwear, like high heels or tight shoes, which unevenly distribute weight onto the forefoot. Additionally, engaging in high-impact activities or having inherent anomalies in foot or toe structure can exacerbate the situation. For example, a longer second metatarsal can increase pressure during walking or running, heightening the risk for capsulitis in the second toe.
Capsulitis tends to affect women between the ages of 30 and 60 more frequently. Your risk of developing this condition might rise if you:
- Work in environments that necessitate frequent tiptoe standing or climbing, or if you spend a lot of time on hard surfaces;
- Experience direct trauma to the joint, such as an upward force applied to the toe in sports activities;
- Suffer from foot irregularities, including bunions, claw toes, or hammertoes;
- Possess tightness in the calf muscles;
- Exhibit instability in the arch of your foot;
- Have forefoot arthritis.
Since the stress each person puts on their feet and joints varies, pinpointing the specific problem through a thorough evaluation is key to devising an effective treatment strategy.
Identifying the Symptoms

Capsulitis typically manifests along with:
- Pain in the affected joint, especially while walking;
- Swelling and warmth;
- Difficulty wearing shoes due to discomfort;
- Redness around the joint;
- Weakness in the area;
- Feeling like you’re walking on a pebble beneath the ball of your foot.
Diagnosing Capsulitis
Your podiatrist can diagnose capsulitis through a physical assessment and examination of the foot in the clinic. In some cases, medical imaging may be required to rule out other causes of foot pain exhibiting similar symptoms but requiring different treatment approaches, such as Morton’s neuroma. Hence, it is crucial not to self-diagnose, as you risk overlooking a serious diagnosis that necessitates a different treatment or urgent care.
Managing and Treating Capsulitis
The key to treating capsulitis is to alleviate the excessive pressure and forces that initially caused the joint injury. A meticulous assessment by a podiatrist is essential to successful treatment, as this enables them to understand all the contributing factors to your injury. Otherwise, you may spend weeks without seeing any improvements due to an incomplete understanding of the problem. Your treatment may include:
- Changing footwear: Switching to shoes that better control foot motion and don’t overload and excessively strain the ball of the foot;
- Offloading the affected joint using custom foot orthotics: These are uniquely designed to effectively redistribute pressure away from the injured joint and distribute it beneath the other joints, significantly relieving pain when walking and aiding the healing process;
- Accelerating joint healing and repair using foot mobilisation therapy: This approach works on stiff or dysfunctional joints to help improve alignment, release tension, and restore better function;
- Temporarily using specially-made pads or strapping to quickly alleviate pain;
- Addressing muscle imbalances (weak/tight muscles) through a custom stretching and strengthening program: Imbalances may contribute to overloading of the forefoot and hence, the development of capsulitis;
- Surgery is not generally recommended for capsulitis.
Ultimately, we aim to deliver top-tier care, and a carefully designed treatment plan tailored to the individual circumstances of each patient. Our podiatrists understand that foot pain is more than just physical discomfort; it severely limits your ability to enjoy life and achieve your goals. All our treatments focus on not only easing your pain but also preventing the problem from recurring in the future. We stay with you every step of the way, providing comprehensive care to help you regain your pain-free life.
Ignoring the Problem: Capsulitis
If left untreated, capsulitis can lead to the destabilisation of the joint, resulting in serious and often irreversible complications. This includes the joint becoming more prominent and, hence, more prone to excess pressure, injury, corns, calluses, and pressure sores. Additionally, the toes might start crossing over one another over time when the joint capsule, responsible for maintaining a healthy alignment, is no longer functioning properly.
Impact and Prevalence of Capsulitis
Capsulitis is more than just a foot discomfort; it’s a pain that can significantly affect a person’s daily life and activities. It can impair mobility and reduce one’s ability to perform basic tasks such as walking, running, or standing for prolonged periods. Understanding its prevalence and impact can help shed light on effective ways to manage and prevent it.
Prevention Tips for Capsulitis

Individuals can prevent capsulitis by wearing supportive shoes that distribute body weight evenly across the foot. Regular foot exercises to strengthen the muscles, maintaining a healthy body weight to reduce pressure on the feet, and seeking early treatment for foot pain are some of the preventive measures. Regular foot checks and assessments can help identify and manage foot abnormalities before they turn into serious condition such as capsulitis.
Frequently Asked Questions
While these terms are often used interchangeably, they refer to different aspects of joint capsule damage. Synovitis is the inflammation of the tissue lining the joint capsule, known as the synovial membrane. This is responsible for producing synovial fluid, which is overproduced in synovitis, leading to added swelling. Capsulitis describes damage to the outer joint capsule, as opposed to its inner lining. The two conditions often coexist.
Conclusion
Understanding the nature and implications of capsulitis is crucial in managing its impact. Being aware of the causes, symptoms, and treatment options can not only help patients navigate their way toward recovery, but it can also assist in the prevention of such painful conditions. Remember, your feet bear the weight of your body daily; giving them the care they deserve is essential for a healthy and active life.
In wrapping up, capsulitis is a painful foot condition that can significantly impact an individual’s quality of life. It is essential to recognize the symptoms early and seek immediate medical attention to prevent any potential complications. With a thorough diagnosis, effective treatment plan, and preventative measures, individuals can manage and overcome capsulitis.
The post Understanding Capsulitis: Causes & Treatments appeared first on PodiAtry NZ.
]]>The post Foot and Knee Pain: Common Symptoms and Treatments appeared first on PodiAtry NZ.
]]>- How is knee pain connected to foot posture and lower limb biomechanics?;
- What are the common causes of knee pain and how do they develop?;
- In what ways does foot posture impact knee health and contribute to knee pain?;
- What are the effective treatment methods available for managing foot and knee pain?;
- How can individuals prevent foot and knee pain through lifestyle and exercise?;
- What role does footwear play in the prevention and management of foot and knee pain?;
- How can stretching and strengthening exercises contribute to the alleviation of foot and knee pain?;
- What is the significance of maintaining a healthy weight in preventing strain and pain in the knees and feet?;
- How does pregnancy affect knee and overall lower limb pain, and what can be done to manage it?;
- When is it advisable to consult a podiatrist for foot and knee pain, and what can one expect from the consultation?
The Connection Between Knee Pain and Foot Posture
Often, knee discomfort is directly linked to foot posture and lower limb biomechanics. In fact, these factors can often be the root cause of the pain. A misaligned foot posture can disrupt your walking pattern, putting extra strain on certain parts of the knee, such as the joints and soft tissues.
In cases where individuals have flat feet or rotational problems, these conditions are likely contributing to knee discomfort. These issues cause the knee to roll inward into an abnormal position while standing, walking, or running. Similarly, individuals with high arches may also encounter knee pain. Insufficient shock absorption due to high arches leads to additional strain on the knee during everyday activities.
Neglecting proper treatment can lead to changes in your gait due to persistent pain. Over time, poor foot posture can cause discomfort or complications in the hips, lower back, and even up to the neck.
Exploring the interconnection between foot and knee pain is crucial in comprehending conditions like capsulitis, which can impact joint health and mobility. You may also like to delve into specific strategies for managing and alleviating the symptoms associated with capsulitis.
Common Causes of Knee Pain
- Bursitis: This condition happens when the tiny, fluid-filled sacs or bursae that act as cushions for the bones, tendons, and muscles around joints become inflamed and swollen due to excess stress or irritation;
- Osgood-Schlatter Disease: Mostly affecting active, sports-loving adolescents in their growth phase, this disease occurs from the inflammation of the area below the knee where the patellar tendon from the kneecap connects to the shinbone;
- Stress Fracture: These are tiny cracks or microfractures in the bone that gradually develop over time, primarily due to overuse or repetitive activity that prevents the bone from healing;
- Osteoarthritis: This condition develops when the smooth, elastic tissue or cartilage that protects the ends of bones wears down over time, causing pain and swelling in the major joints and making them difficult to move;
- Iliotibial Band Syndrome: This painful condition occurs when the band running down the exterior of your thigh and connecting your hip to your knee becomes overused or overloaded;
- Pregnancy: Pregnancy can cause various aches and issues not just in the feet but throughout the body. Hence, many pregnant women also experience knee pain, lower back pain, hip pain, ankle pain, and more.
Understanding the Impact of Foot Posture on Knee Pain

It’s essential to understand the impact of foot posture on knee health in managing and preventing knee pain. Both flat feet and high-arched feet can contribute to knee pain by causing an imbalance in the distribution of pressure on the knees. This imbalance can lead to strain on the knee joints and soft tissues, resulting in pain and discomfort.
Effective Treatment Methods for Foot and Knee Pain
There are numerous treatments available for foot and knee pain. From physiotherapy and exercise to certain medications and in some extreme cases, surgery. Choosing the right treatment depends largely on the cause of the pain. Consulting with a podiatrist can help determine the right course of treatment.
Prevention Tips for Foot and Knee Pain
Preventing foot and knee pain involves maintaining proper foot posture, strength and stability. This can be achieved by:
- Wearing proper footwear that provides good arch and heel support;
- Stretching and strengthening exercises for feet and knees;
- Regular low impact exercises like swimming or biking;
- Maintaining a healthy weight to reduce strain on knees and feet.
Conclusion
Understanding the connection between foot posture and knee pain is crucial in both treatment and prevention of these common issues. By understanding the causes and being proactive in prevention methods, it’s possible to reduce the frequency and severity of foot and knee pain. Always consult with a healthcare professional or podiatrist for personalized guidance and treatment.
The post Foot and Knee Pain: Common Symptoms and Treatments appeared first on PodiAtry NZ.
]]>The post Foot Troubles in Kids: Understanding Growing Pains appeared first on PodiAtry NZ.
]]>- What are growing pains in children, and what causes them?;
- How can one recognize the symptoms of growing pains in children?;
- What are the specific conditions related to growing pains, such as Sever’s Disease and Osgood-Schlatter Disease?;
- At what age are children most likely to experience growing pains, and can they extend into the teenage years?;
- What methods are used for diagnosing growing pains in children?;
- What are some effective at-home strategies for managing and alleviating growing pains?;
- How can professional podiatry support assist in the treatment of growing pains?;
- What preventative strategies can reduce the risk of growing pains in children?;
- What is the range of pediatric foot and leg conditions, and how can they be managed comprehensively?;
- Why is it important not to dismiss growing pains as a normal part of growth, and what steps can be taken for improvement?
Managing growth-related discomfort isn’t merely about alleviating immediate pain and inconvenience for young ones; it also involves ensuring they don’t have to sideline their cherished activities and time with friends.
Growth-related discomfort typically manifests in children aged 3 to 12 years, frequently coinciding with periods of rapid growth. Contrary to widespread belief, these pains are not an inevitable aspect of childhood that must be endured until they naturally subside. In reality, musculoskeletal pain always has an underlying cause, and pinpointing this cause allows for a clear and effective treatment strategy.
If you’re experiencing foot and knee pain, you may also like to explore effective remedies and preventive measures in our comprehensive article on foot and knee pain management.
Understanding Growing Pains: Origins and Mechanisms
Growing pains are a phenomenon tied to the development and enlargement of our bones and muscles. During the phase before bones reach full maturity, they contain areas known as ‘growth plates’—cartilaginous zones that serve as sites for new bone cell development, facilitating bone growth. These growth plates are less robust than the surrounding bone structure, rendering them more susceptible to discomfort under strain.
As the body grows, so do the muscles, undergoing periods of elongation and strengthening. This process sometimes involves periods of tightness as the muscles adjust to keep pace with the body’s overall growth. Muscles are connected to bones, and their movement exerts tension on these bones. When children engage in physical activity, this tension affects the growth plates, leading to irritation and discomfort. This reaction is the genesis of growing pains, which persist until the muscle and tendon-induced tension on the bone diminishes and stabilizes.
Identifying Symptoms of Growing Pains in Children
Episodes of growing pains can occur frequently, affecting around 43% of children who may experience attacks at least once a week, with some enduring daily discomfort for over six months. If your child is undergoing growing pains, watch out for these signs:
- Complaining of pain during or after physical activities, which usually eases with rest;
- Noticing that specific movements or positions of their feet and legs can either worsen or alleviate the symptoms;
- Waking up in the middle of the night due to pain;
- Exhibiting a limp after engaging in sports or physical activities;
- Displaying symptoms such as throbbing, redness, or swelling at the affected growth plate.
Sever’s Disease: Growing Pains in the Heels

Growing pains affecting the back of the heels are often attributed to Sever’s Disease. This condition arises when a tight Achilles tendon, connecting to the heel bone, tugs and inflames the growth plate located at the back of the heel. Given the significant force exerted by the Achilles tendon, especially during activities like running, this area is particularly prone to such discomfort. Despite its name, Sever’s Disease is not an illness but a treatable condition.
Osgood-Schlatter Disease: Growing Pains in the Knees
Growing pains manifesting in the knees may indicate Osgood-Schlatter Disease. This condition occurs when the tendon descending from the thighs and passing over the knee to attach at the top of the shin bone (tibia) irritates the nearby growth plate, leading to knee discomfort. Any actions involving knee bending, such as squatting or running, can trigger pain due to the stretching of this tendon. Medically termed Osgood-Schlatter disease, it is manageable with appropriate treatment.
Iselin’s Disease: Midfoot Growing Pains
Iselin’s Disease, characterized by growing pains in the midfoot region, targets the middle of the foot, particularly along the outer edge. This discomfort stems from irritation to the growth plate situated at the base of the fifth metatarsal, identifiable by a natural bony protrusion. The culprit behind this irritation is the peroneus brevis tendon.
Kohler Disease: A Concerning Foot Condition
Kohler Disease presents as pain, redness, and swelling centered around the navicular bone in the foot. Primarily affecting children aged between five and ten years, it results from a disruption in the foot’s blood supply, leading to potential bone damage, fracture, or collapse before eventual healing and solidification. While rare, if your child experiences discomfort in this area, prompt consultation with a podiatrist is essential.
Freiberg’s Infarction: Foot Bone Complications
Freiberg’s Infarction refers to the premature demise of bone tissue, commonly occurring at the head of the second metatarsal bone in the foot due to compromised blood supply. Typically afflicting children or teenagers in their early teens, symptoms may include foot ball pain, stiffness, swelling, and discomfort when bearing weight. If these symptoms arise, seeking professional podiatric care is crucial.
Growth Pain Age Range in Kids & Teens
Growing pains are most commonly experienced by children aged 3 to 12 years. However, individual variations in growth and development mean that some children and adolescents may encounter these pains at different stages, extending into their teenage years.
Diagnosis of Growing Pains in Children
The diagnosis of growing pains in children involves a holistic method that starts with a detailed conversation to understand the nature and patterns of their discomfort, including the onset of pain, factors that exacerbate it, and their daily physical activities. A thorough physical examination follows, aimed at identifying the source of the pain. This examination also includes a process to rule out other potential causes, such as muscle or tendon injuries. This comprehensive diagnostic approach helps in accurately determining the underlying issue, facilitating the recommendation of an effective treatment plan.
Managing and Alleviating Growing Pains: Strategies for Relief
Growing pains, while often resolving over time, can be a source of discomfort, potentially affecting a child’s participation in sports and physical activities. Strategies to manage these pains include implementing simple changes at home and consulting a podiatrist for a personalized treatment plan, aimed at ensuring children remain active and comfortable.
At Home Strategies:
- Applying ice packs to the affected area before and after physical activity for 10-15 minutes can mitigate discomfort;
- Ensuring children wear comfortable, supportive, and well-fitting shoes, and avoiding walking barefoot can provide necessary support and reduce pain;
- Daily stretching exercises tailored to the pain location can alleviate discomfort;
- Gentle muscle massage may also offer relief.
Professional Podiatry Support:
Podiatrists specialize in devising customized treatment plans to address and relieve growing pains, facilitating a child’s return to their preferred activities. Treatment strategies may include:
- Custom foot orthotics to correct alignment issues and support affected bones and tendons;
- Stretching and strengthening exercises to ease tendon strain and address muscle imbalances;
- Footwear assessments to identify and rectify any aggravating factors, recommending shoes that provide better support and alignment;
- Modifications to physical activities to encourage active recovery, including low-impact exercises that do not exacerbate the pain;
- Use of padding, strapping, and percussive therapy (e.g., Theragun) for immediate relief and support during activity, while waiting for more permanent solutions such as orthotics.
These approaches aim to reduce the impact of growing pains on daily life, ensuring children can continue engaging in sports and activities without significant discomfort.
Strategies for Mitigating the Risk of Growing Pains in Children
Reducing the likelihood of growing pains in children can be achieved through a series of proactive measures. Encouraging children to engage in thorough warm-up exercises before participating in sports activities can significantly help in loosening their muscles, thereby minimizing the risk of discomfort. Monitoring and aiding in the maintenance of proper sports techniques is also crucial in preventing unnecessary stress on their developing bodies. It may be beneficial to limit participation in sports that specifically exacerbate pain in sensitive areas, thus avoiding the triggering of painful symptoms. Furthermore, ensuring that children wear supportive and well-fitted shoes designed with adequate shock absorption can provide essential support to their growing bodies, thereby contributing to the prevention of growing pains.
Comprehensive Care for Pediatric Foot and Leg Conditions

A broad spectrum of foot and leg issues in children is addressed and managed, covering conditions from common to complex. These include:
- In-toeing and out-toeing adjustments;
- Correction for knock knees and bow legs;
- Management of shin splints;
- Solutions for toe walking;
- Treatment for ankle sprains;
- Remedies for hammertoes;
- Removal of plantar warts;
- Care for ingrown toenails;
- Approaches to manage pain associated with hypermobility;
- Alleviation of tired, achy legs.
Identifying foot and leg problems in children can be challenging, particularly if they do not express discomfort. It’s advisable to seek a professional foot evaluation for children exhibiting signs such as:
- Unusual walking patterns;
- Frequent tripping and falling;
- Difficulty keeping pace with peers during physical activities;
- Skin rashes between toes;
- Discoloration or pain associated with toenails, potentially indicating ingrown toenails;
- Shoes showing uneven wear patterns;
- Limping or favoring one leg;
- Noticeable foot or leg misalignments;
- Presence of hard skin lumps or bumps.
Conclusion
Growing pains, while common, should never be dismissed as a normal part of growth. Understanding the cause of these pains is the first step to providing relief to children. By seeking professional advice and implementing healthy habits, a child’s experience of growing pains can be significantly improved.
Growing pains in children, while common, should never be dismissed as mere side effects of childhood growth. There are in-depth explanations and effective solutions for these pains. In understanding the cause of these aches, parents and caregivers can better assist in providing relief to children. With the right blend of professional help and implementing healthy habits at home, a child’s experience of growing pains can be significantly alleviated. It’s important that children continue to engage in the activities they love, without the hindrance of growing pains.
FAQs
Active children may exert more stress on their developing bones, which can lead to growing pains. However, a lack of physical activity does not prevent growing pains from occurring.
The duration of growing pains varies; they can last from a few weeks to months, or in some cases, years.
Differentiating between growing pains and injuries can be complex since traumatic injuries are usually associated with a distinct event, while overuse injuries and growing pains develop gradually. A definitive diagnosis typically requires evaluation by a specialist, such as a podiatrist.
Children as young as 2 years old can be evaluated by a podiatrist for foot and leg health concerns.
Flat feet can elevate the risk of foot and leg pain and related issues, including growing pains. However, if a child with flat feet is not experiencing pain or other problems, treatment may not be necessary at a young age.
The post Foot Troubles in Kids: Understanding Growing Pains appeared first on PodiAtry NZ.
]]>The post Understanding Down Syndrome Foot Challenges appeared first on PodiAtry NZ.
]]>Typically, people with Down syndrome are recognized by distinct physical traits such as reduced stature, an upward slant to the eyes, decreased muscular tonality, and a single crease across the palm. However, less commonly known is that this condition can also precipitate a variety of foot-related problems.
Key Questions Addressed in this Article:
- What are the common foot deformities experienced by individuals with Down syndrome?;
- How do foot issues impact mobility and overall well-being in individuals with Down syndrome?;
- What are the challenges related to shoe fitting for individuals with Down syndrome?;
- How are gait abnormalities influenced by Down syndrome and foot deformities?;
- What role does physical therapy play in addressing gait abnormalities in individuals with Down syndrome?;
- What orthotic management options are available to improve comfort and functionality for individuals with Down syndrome?;
- When are surgical interventions considered for severe foot deformities in individuals with Down syndrome?
Understanding Foot Challenges for Individuals with Down Syndrome
There are several common foot-related complications experienced by those with Down Syndrome, which can be broadly classified into three categories:
- Foot Abnormalities: The structure of the foot can showcase several anomalies, such as a widened forefoot, progressive bunions, claw toes, and hammer toes. Additional deformities may include webbing between the second and third toes, increased spacing between the first and second toes, loosened ligaments, and a flattened foot posture. These structural deviations can lead to other complications such as plantar fasciitis-induced heel pain and knee discomfort;
- Footwear Fitting Problems: The unique foot structure, characterized by broad and flat contours, can make it challenging to find appropriately fitting shoes. Recent studies identified that among a group of 48 children and adolescents with Down syndrome, nearly 62% were wearing shoes that were excessively long, while approximately 60% wore shoes that were too narrow. Incorrectly fitted footwear can exacerbate foot discomfort, cause skin irritations, and accelerate the progression of foot deformities;
- Skin Complications: Frequent skin issues include corns and calluses, excessive moisture between toes leading to skin damage, excessive dryness, thickened toenails, ingrown toenails, and fungal nail infections.
Furthermore, reduced muscle tonicity (hypotonia) may result in the feet and legs feeling fatigued and sore by the end of the day.
How Does Down Syndrome Affect Gait?
Altering the way a person walks, or their gait, is one of the significant challenges faced by individuals with Down Syndrome. Distinct characteristics of Down syndrome, such as a different foot shape and reduced muscle tone, significantly contribute to this.
Several other factors that directly influence their gait include a limited range of ankle movement, exaggerated hip flexion, and outward rotation, alongside a propensity for toe-walking. These elements can negatively affect their balance, potentially leading to a higher frequency of stumbling and falls due to foot-dragging during ambulation.

Down Syndrome Foot Issues: How Can They Be Managed?
We begin with a detailed assessment of the feet and legs, taking into account the daily life challenges and individual goals of the patient. Based on this information, we formulate a custom-tailored course of action, which may include:
- Routine Skin and Nail Maintenance: Regular appointments facilitate the management of corns, calluses, and thickened nails, significantly reducing discomfort. We also proactively address factors contributing to their rapid progression, putting preventive measures in place;
- Footwear Modifications and Recommendations: We pride ourselves on offering a variety of shoe modification options tailored to current symptoms and comfort levels. We also provide custom footwear and recommendations for wider and supportive shoes to accommodate mild foot changes;
- Custom Foot Orthotics: In light of the detailed assessment and 3D foot scan, we develop unique custom foot orthotics. These come with specific functions such as offloading painful areas and providing additional ankle support. They replace your shoe liner, offering superior comfort and support with every step. We prioritize selecting lightweight orthotic materials that don’t burden the feet, considering the lower muscle tone;
- Ankle-Foot Orthoses (AFO): In certain instances, custom AFOs may be used instead of foot orthoses. They provide similar benefits and extend above the ankle for enhanced stability, especially in cases of greater weakness;
- Surestep SMO: The Surestep supramalleolar orthoses (SMO) is an innovative solution for children with low muscle tone due to Down syndrome. When paired with suitable Surestep footwear, it can significantly enhance their mobility and independence;
- Ingrown Toenail Surgery: For recurrent and painful ingrown nails, a corrective surgery may be performed to permanently solve the problem;
- Injury Management: Owing to the increased risk of injuries in Down Syndrome, we manage issues such as heel pain using our proven protocols, factoring in the unique circumstances of each individual.
Conclusion
In conclusion, understanding the unique foot challenges faced by individuals with Down syndrome, including conditions like Morton’s Neuroma, is essential for providing comprehensive care and improving quality of life. By addressing foot deformities, shoe fitting issues, and gait abnormalities through a multidisciplinary approach encompassing orthotic management, physical therapy, and surgical interventions when necessary, healthcare professionals can optimize outcomes and enhance mobility for individuals with Down syndrome. Through tailored treatment strategies and ongoing support, it is possible to mitigate the impact of foot issues and empower individuals with Down syndrome to lead active and fulfilling lives.
The post Understanding Down Syndrome Foot Challenges appeared first on PodiAtry NZ.
]]>The post Morton’s Neuroma: A Guide appeared first on PodiAtry NZ.
]]>Key Questions Addressed in this Article:
- What exactly is Morton’s Neuroma, and what are the factors contributing to its development?;
- What are the causes and risk factors associated with Morton’s Neuroma?;
- What are the common symptoms of Morton’s Neuroma?;
- How is Morton’s Neuroma diagnosed, and what are the differential diagnoses to consider?;
- What are the treatment options available for Morton’s Neuroma?;
- What can happen if Morton’s Neuroma is ignored?;
- How can Morton’s Neuroma be prevented?;
- Why is early recognition and management of Morton’s Neuroma important for foot health and mobility?
What is Morton’s Neuroma?
Morton’s neuroma develops in the plantar digital nerves that run between the long bones of the foot. The condition arises due to compression and friction trauma on the surrounding tissue, leading to chronic thickening and swelling of the nerve lining located between the toes. This thickened bulbus in the inflamed nerve is known as Morton’s neuroma, typically causing pain in the ball of the foot. While it commonly occurs between the third and fourth toes, it can also manifest in other toe joint spaces.
Causes & Risk Factors
The primary cause of Morton’s neuroma is tight and poorly fitting footwear, particularly high heels, which irritate and compress the nerves in the feet. The pressure exerted by cramming toes into narrow or tapered toe boxes, along with the added strain from the sloping shape of high heels, contributes to nerve irritation. Foot and gait abnormalities, such as abnormal joint mobility and range of motion, can also increase pressure on the ball of the foot. Activities involving repetitive stress on the foot, like running or court sports, may further aggravate these nerves.
Symptoms
Progressive Discomfort
As Morton’s neuroma advances, the pain and discomfort can become more persistent and intense. Walking or standing for extended periods may exacerbate the symptoms, leading to aching or shooting pains in the affected area. Some individuals may notice a visible swelling or thickening between the toes, accompanied by a feeling of instability or a clicking sensation when walking.
Impact on Mobility
The presence of Morton’s neuroma can significantly impact mobility and quality of life. Individuals may find it challenging to engage in physical activities or wear certain types of footwear comfortably. The pain and discomfort associated with the condition can limit daily activities and lead to a decreased range of motion in the foot.
Diagnosis
Clinical Evaluation
Diagnosing Morton’s neuroma typically involves a thorough clinical evaluation by a healthcare provider. The medical history of the individual, including details about symptoms and potential risk factors, is assessed. A physical examination of the foot is conducted to identify areas of tenderness, swelling, or abnormal sensations. Palpation of the foot may elicit pain or a clicking sensation, providing valuable diagnostic clues.
Imaging Studies
In some cases, imaging studies such as X-rays, ultrasound, or magnetic resonance imaging (MRI) may be recommended to visualize the structures of the foot in greater detail. These imaging modalities can help confirm the presence of a Morton’s neuroma, assess its size and location, and rule out other potential causes of foot pain. Imaging findings, combined with clinical observations, aid in formulating an accurate diagnosis and treatment plan.
Differential Diagnosis
Distinguishing Morton’s neuroma from other conditions that cause foot pain is essential for appropriate management. Conditions such as metatarsalgia, stress fractures, bursitis, or arthritis can present with similar symptoms and must be considered during the diagnostic process. Healthcare providers use a combination of clinical assessment, imaging studies, and sometimes nerve conduction tests to differentiate between these conditions and ensure proper treatment.
Treatment
Conservative Approaches
Initial treatment for Morton’s neuroma often involves conservative measures aimed at alleviating symptoms and reducing nerve irritation. These approaches may include wearing supportive footwear with a wide toe box, using orthotic inserts to cushion and support the foot, and avoiding high heels or tight shoes that exacerbate discomfort. Physical therapy exercises focusing on strengthening the foot muscles and improving flexibility can also be beneficial.
Medications
In some cases, nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid injections may be prescribed to reduce pain and inflammation associated with Morton’s neuroma. NSAIDs help alleviate discomfort, while corticosteroid injections deliver targeted relief by reducing swelling around the affected nerve. These medications are typically used in conjunction with other conservative treatments to manage symptoms effectively.
Surgical Intervention
When conservative measures fail to provide adequate relief or if the condition progresses, surgical intervention may be considered. Surgical procedures for Morton’s neuroma aim to release pressure on the affected nerve and remove any thickened tissue causing compression. Depending on the size and location of the neuroma, surgical options may include nerve decompression, neurectomy (nerve removal), or ligament release. Surgical outcomes vary, and individuals undergoing these procedures should discuss the risks and benefits with their healthcare provider.
What Can Happen If I Ignore Morton’s Neuroma?
Progression of Symptoms
Ignoring the signs of Morton’s neuroma can lead to the progression of symptoms and worsening discomfort over time. Untreated neuromas may increase in size and become more painful, impacting daily activities and mobility. Continued pressure and irritation on the nerves can result in chronic inflammation and structural changes within the foot, potentially leading to long-term complications.
Functional Limitations
Persistent Morton’s neuroma can cause functional limitations and affect quality of life. Individuals may experience difficulty walking, standing, or participating in physical activities due to ongoing pain and discomfort. The condition can interfere with footwear choices, work responsibilities, and recreational pursuits, limiting overall mobility and independence.
Risk of Complications
Prolonged neglect of Morton’s neuroma raises the risk of developing secondary complications. Chronic nerve compression and inflammation can lead to nerve damage, altered sensation in the foot, and potential gait abnormalities. Severe cases of untreated Morton’s neuroma may require more extensive interventions and have a greater impact on foot function and overall well-being.

Prevention
Footwear Selection
Choosing appropriate footwear plays a crucial role in preventing Morton’s neuroma. Opt for shoes with a roomy toe box that allows for natural toe splay and minimizes pressure on the forefoot. Avoid high heels or shoes with narrow, pointed toe boxes that compress the toes and increase the risk of nerve irritation. Selecting supportive footwear with adequate cushioning and arch support can help maintain foot health and reduce the likelihood of developing neuromas.
Foot Care Practices
Practicing good foot hygiene and care can contribute to overall foot health and reduce the risk of neuroma development. Keep feet clean and dry, trim toenails properly to prevent ingrown nails, and inspect the feet regularly for any signs of irritation or injury. Maintaining a healthy weight, engaging in regular physical activity, and stretching the feet and lower limbs can also promote foot health and minimize the impact of biomechanical stressors on the feet.
Conclusion
In conclusion, recognizing the signs and symptoms of Morton’s neuroma and heel pain is essential for timely diagnosis and effective treatment. By understanding the causes, risk factors, symptoms, diagnostic approaches, treatment options, potential consequences of neglecting the condition, preventive measures, and the importance of proactive foot care, individuals can take proactive steps to maintain foot health and mobility.
The post Morton’s Neuroma: A Guide appeared first on PodiAtry NZ.
]]>